Understanding Secondary Hypogonadism
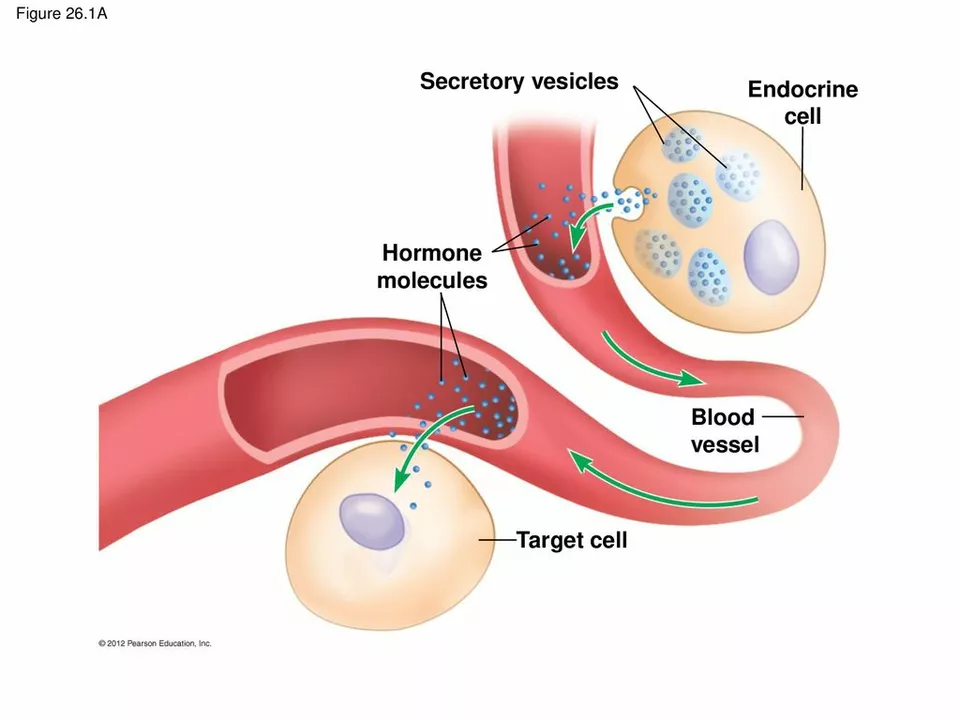
Before diving into the relationship between secondary hypogonadism and prostate health, it's crucial to understand what secondary hypogonadism is. Secondary hypogonadism, also known as hypogonadotropic hypogonadism, is a condition in which the testes do not produce enough testosterone, a hormone responsible for the growth and development of male sexual characteristics. This condition can result from problems with the hypothalamus or pituitary gland, which control hormone production in the body.
Secondary hypogonadism can affect men of any age and can have various causes, including genetic disorders, tumors, infections, or even certain medications. Symptoms of this condition can range from reduced sex drive, erectile dysfunction, decreased muscle mass, and increased body fat, among others. As we delve deeper into the topic, we will explore the potential impact of secondary hypogonadism on prostate health.
Prostate Health: An Overview
The prostate is a small, walnut-shaped gland found in men, located just below the bladder and surrounding the urethra. It plays a vital role in male reproductive health, as it produces and secretes seminal fluid, which nourishes and transports sperm during ejaculation. Maintaining optimal prostate health is crucial for men, as issues with this gland can lead to various health problems, including prostatitis (inflammation of the prostate), benign prostatic hyperplasia (BPH), and prostate cancer.
Several factors can contribute to poor prostate health, such as age, genetics, lifestyle choices, and hormonal imbalances. This article will focus on the link between secondary hypogonadism and prostate health, examining how low testosterone levels can impact this essential gland.
The Role of Testosterone in Prostate Health
Testosterone plays a significant role in maintaining prostate health. It supports the growth and development of the prostate gland during puberty and helps maintain its normal function throughout adulthood. Testosterone also regulates the production of dihydrotestosterone (DHT), a hormone that can stimulate prostate growth and has been implicated in BPH and prostate cancer.
As such, imbalances in testosterone levels, such as those seen in secondary hypogonadism, may have a direct impact on prostate health. In the following sections, we will discuss some of the potential consequences of low testosterone on the prostate and how they may manifest in individuals with secondary hypogonadism.
Secondary Hypogonadism and Benign Prostatic Hyperplasia (BPH)
Benign prostatic hyperplasia, or BPH, refers to the non-cancerous enlargement of the prostate gland. This condition can cause urinary symptoms like frequent urination, weak urine stream, and difficulty emptying the bladder. Research has shown that men with secondary hypogonadism may be at an increased risk of developing BPH due to the hormonal imbalances associated with their condition.
Low testosterone levels can lead to an increase in the conversion of testosterone to DHT, which in turn can stimulate prostate growth. This can result in an enlarged prostate, causing the urinary symptoms commonly associated with BPH. It is crucial for men with secondary hypogonadism to monitor their prostate health closely and discuss any concerns with their healthcare provider.
Secondary Hypogonadism and Prostatitis
Prostatitis is a condition characterized by inflammation of the prostate gland, which can cause pain, urinary problems, and sexual dysfunction. While the exact cause of prostatitis remains unclear, hormonal imbalances, such as those seen in secondary hypogonadism, have been implicated as potential contributing factors.
Studies have suggested that men with low testosterone levels may be more susceptible to developing prostatitis, possibly due to the impact of hormonal imbalances on the immune system and inflammatory responses. This highlights the importance of addressing and managing secondary hypogonadism to maintain overall prostate health and reduce the risk of prostatitis.
Secondary Hypogonadism and Prostate Cancer
Prostate cancer is the most common cancer among men, and its development has been linked to various factors, including age, genetics, and hormonal imbalances. While the relationship between secondary hypogonadism and prostate cancer is complex and not fully understood, some studies have suggested that low testosterone levels may be associated with an increased risk of prostate cancer.
It is essential to note that the relationship between testosterone and prostate cancer remains a topic of ongoing research and debate within the scientific community. Men with secondary hypogonadism should work closely with their healthcare providers to monitor their prostate health and discuss any concerns or potential risk factors related to their condition.
Treatment Options for Secondary Hypogonadism and Prostate Health
For men with secondary hypogonadism, addressing the underlying cause of their low testosterone levels is often the first step in improving their prostate health. This may involve changes in medication, treatment of underlying medical conditions, or hormone replacement therapy (HRT) to restore testosterone levels to a more normal range.
It is important to note that testosterone replacement therapy can have varying effects on prostate health, and its use in men with pre-existing prostate conditions should be carefully considered and monitored by a healthcare provider. In some cases, additional treatments or interventions may be necessary to address prostate-related issues that arise as a result of secondary hypogonadism.
Preventative Measures for Prostate Health in Men with Secondary Hypogonadism
While it may not be possible to prevent secondary hypogonadism or its impact on prostate health entirely, there are several steps men can take to promote overall prostate health and reduce their risk of developing prostate-related issues:
- Maintain a healthy diet rich in fruits, vegetables, and whole grains
- Exercise regularly to promote overall health and well-being
- Maintain a healthy weight
- Avoid smoking and excessive alcohol consumption
- Discuss any concerns about prostate health with a healthcare provider and undergo regular prostate screenings as recommended
By taking these preventative measures and working closely with their healthcare providers, men with secondary hypogonadism can help protect their prostate health and reduce their risk of developing prostate-related issues.

Sharon M Delgado
I just read this and had to pause... seriously, who knew low testosterone could mess with your prostate like this? I mean, I knew it affected libido, but prostate growth? DHT? I need to talk to my doctor.
Also, why is this not common knowledge? My mom’s a nurse and she’s never mentioned this. We need better public health messaging.
Paul Orozco
This article is overly academic and lacks any practical clinical insight. The references are from PubMed, yes, but where is the meta-analysis? Where are the longitudinal studies? The tone is alarmist without sufficient evidence to support causality. One cannot infer that low testosterone causes prostate cancer merely because both occur in aging men. Correlation is not causation. This is medical misinformation dressed as education.
Bobby Marshall
Man, this hit different. I’ve been dealing with low T since my late 30s-fatigue, mood swings, the whole shebang-and last year my PSA spiked. My urologist didn’t blink, just said, ‘Let’s watch it.’ Reading this made me feel less alone.
It’s wild how your body keeps secrets until it doesn’t. I started lifting again, cut out soda, and now I sleep like a baby. Not cured, but I’m not scared anymore. If you’re reading this and feeling lost-reach out. You’re not broken. You’re just under-served by the system.
Ardith Franklin
Let’s be real-this whole ‘testosterone = prostate danger’ narrative is a pharmaceutical distraction. Big Pharma doesn’t want you to know that BPH is mostly caused by sitting too much, eating processed food, and drinking too much coffee. They sell you HRT to keep you dependent. And don’t get me started on PSA tests-false positives everywhere. Your prostate isn’t the enemy. The system is.
Jenny Kohinski
This was so helpful 😊 I’ve been researching this for my dad-he’s 62 and just got diagnosed with secondary hypogonadism. He’s scared to start HRT because he’s heard it ‘causes cancer.’ Now I can actually explain to him that it’s not that simple.
Thank you for breaking it down so clearly! I’m sharing this with his doctor’s office. Maybe they’ll finally stop treating him like a statistic 💙
Aneesh M Joseph
Nah this is all fake science. Testosterone doesn’t cause BPH. I read on a forum that it’s actually estrogen that’s the problem. Also, prostate cancer is caused by 5G towers. My cousin’s neighbor’s dog had it and never took HRT. So yeah.
Deon Mangan
Ah yes, the classic ‘hormones are magic’ narrative. Let me summarize: low T → more DHT → prostate swells → panic.
Meanwhile, 70% of men over 70 have BPH and 90% of them have normal testosterone. So… maybe it’s not the T? Maybe it’s just… aging? Or maybe your prostate is a stubborn old man who refuses to shrink no matter what you feed him?
Also, PSA is a terrible test. Don’t let your doctor scare you into a biopsy because your number is 4.2. That’s not a death sentence. That’s a Tuesday.
PS: I’m a urologist. Yes, I’m sarcastic. No, I won’t prescribe you testosterone unless you’ve tried lifestyle changes. And yes, I’ve seen men get better by biking more and drinking less beer. 🍻