Stapedectomy: What It Is, Who Needs It, and What to Expect
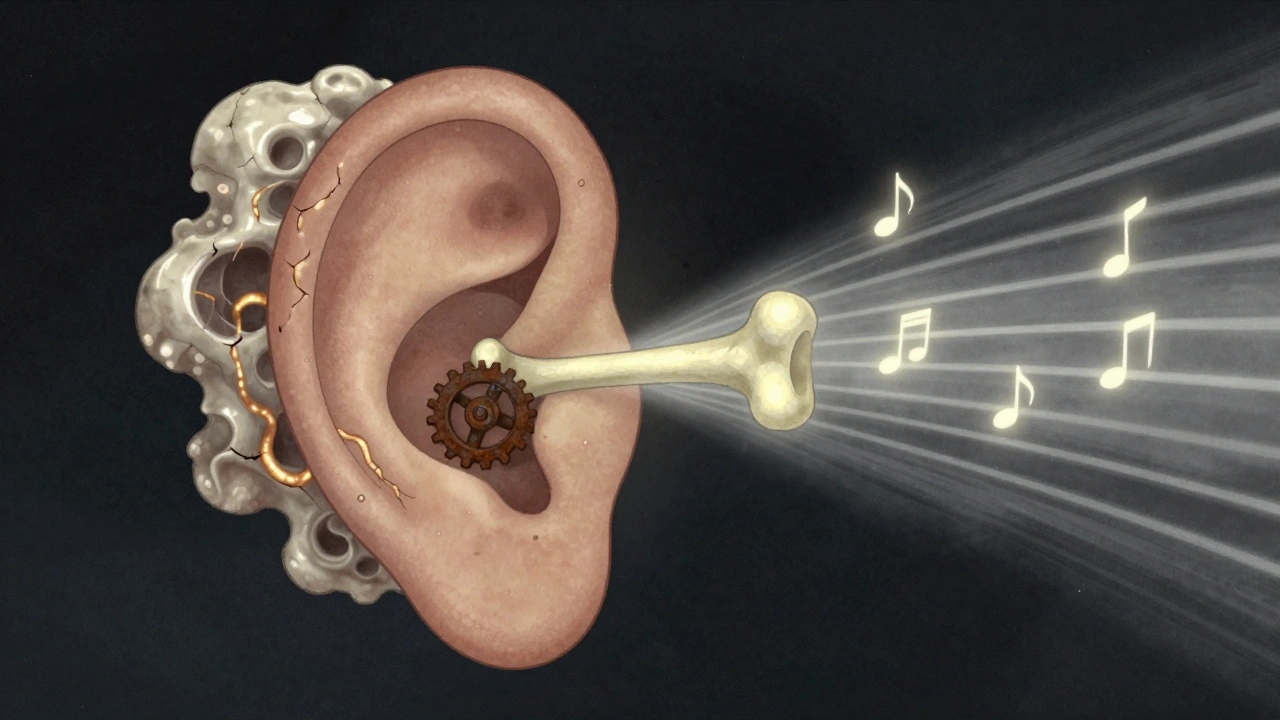
When hearing fades slowly over time—especially in one ear—it’s often not just aging. It could be otosclerosis, a condition where abnormal bone growth around the stapes bone in the middle ear blocks sound transmission. Also known as fixed stapes, it’s one of the most common causes of conductive hearing loss in young adults. That’s where stapedectomy, a precise surgical procedure to replace the immobilized stapes bone with a prosthetic device comes in. This isn’t brain surgery, but it’s delicate: the stapes is the smallest bone in your body, and the surgery happens right next to the inner ear, where balance and hearing meet.
Stapedectomy doesn’t fix all hearing loss. It’s targeted. If your hearing test shows a conductive loss—meaning sound can’t travel properly through the middle ear—and imaging confirms otosclerosis, this surgery can restore hearing by up to 90% in many cases. But it’s not for everyone. If you have sensorineural hearing loss from nerve damage, or if your otosclerosis is too advanced, the risks outweigh the benefits. Your doctor will check your ear anatomy, your overall health, and even your lifestyle—like whether you’re a scuba diver or work in loud environments—before recommending it.
What happens during the procedure? A tiny incision is made in the ear canal. The surgeon lifts the eardrum, removes the fixed stapes, and inserts a tiny piston-like prosthesis—often made of titanium or platinum—that connects the incus bone to the inner ear. The eardrum is put back, and you’re usually home the same day. Recovery takes a couple of weeks. You’ll feel some dizziness at first, and your ear might pop or feel blocked. That’s normal. But if you lose more hearing, have severe vertigo, or notice fluid leaking from your ear, you need to call your doctor right away.
Many people don’t realize that stapedectomy is one of the oldest and most successful ear surgeries still in use today. It’s been refined over 70 years, and modern techniques use microscopes and minimally invasive tools to reduce complications. Still, it’s not risk-free. Rare side effects include taste changes (because a nerve runs near the surgery site), tinnitus, or even permanent hearing loss. That’s why choosing an experienced otolaryngologist matters more than the hospital.
After surgery, most patients notice improved hearing within a few weeks. Some even hear birds singing again, or their own voice without that muffled feeling. But hearing aids are still an option if surgery isn’t right for you. And if you’ve had a stapedectomy, you’ll need to avoid flying or diving until your doctor says it’s safe—pressure changes can mess with the prosthesis.
Below, you’ll find real patient stories, doctor insights, and clear comparisons between stapedectomy and other hearing solutions. Whether you’re considering the surgery, recovering from it, or just trying to understand why your hearing changed, these posts give you what you need—no fluff, no jargon, just facts.
Otosclerosis: What It Is, How It Affects Hearing, and What You Can Do
Otosclerosis is a common cause of hearing loss in adults under 50, caused by abnormal bone growth in the middle ear. Learn how it affects hearing, who’s at risk, and what treatments-including surgery and hearing aids-can restore your hearing.
More