Respiratory Depression: Causes, Risks, and Medications That Can Trigger It
When your breathing slows down too much—so much that your body can’t get enough oxygen—it’s called respiratory depression, a life-threatening condition where the brain fails to signal the lungs to breathe properly. Also known as hypoventilation, it’s not just about feeling sleepy—it’s when your oxygen levels drop low enough to damage organs or stop your heart. This isn’t rare. It happens most often with opioids, pain medications like oxycodone, morphine, and fentanyl that calm the brain’s breathing center, but also with benzodiazepines, sleep aids and anti-anxiety drugs like diazepam or alprazolam, and even when these are mixed with alcohol or other sedatives.
People often don’t realize how quickly this can happen. A single extra pill, combining meds without checking with a doctor, or even just having sleep apnea while on opioids can push breathing into danger. That’s why central sleep apnea, a type of sleep disorder where the brain doesn’t send proper signals to breathe during sleep is such a big concern when opioids are involved. Studies show people with sleep apnea who take opioids have up to three times the risk of nighttime oxygen drops that can lead to hospitalization—or worse. And it’s not just pain meds. Some antidepressants, muscle relaxants, and even certain antihistamines can add up and slow breathing, especially in older adults or those with lung conditions.
You don’t need to be addicted to opioids to be at risk. Even someone taking them exactly as prescribed can develop respiratory depression if they’re also on a sleep aid, drinking alcohol, or have untreated sleep apnea. The real danger? The symptoms sneak up. You might feel drowsy, then dizzy, then your lips turn blue, and suddenly, you’re not breathing enough. That’s why knowing the signs matters more than ever.
Below, you’ll find real-world stories and expert breakdowns on how common medications—like those used for pain, anxiety, or sleep—can quietly suppress breathing. You’ll learn which combinations are most dangerous, how to spot early warning signs, and what steps you can take to protect yourself or someone you care about. This isn’t theoretical. These are the cases that end up in emergency rooms every day. Let’s make sure you’re not one of them.
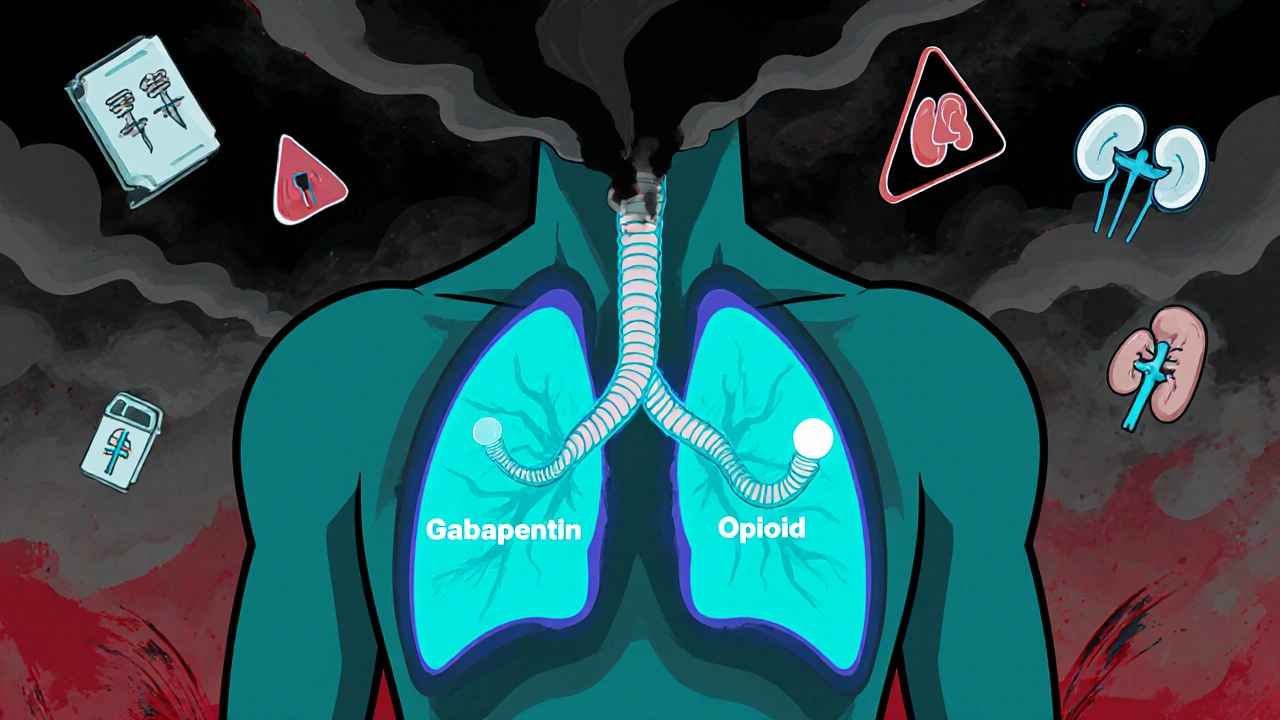
Gabapentinoids and Opioids: The Hidden Danger of Combined Respiratory Depression
Combining gabapentinoids with opioids can dangerously slow breathing-even kill. Learn why this interaction is deadlier than many doctors realize, who’s at risk, and what safer alternatives exist.
More