Respiratory Depression Risk Calculator
This tool helps you understand your risk of respiratory depression when taking gabapentinoids (gabapentin, pregabalin) with opioids or other central nervous system depressants. Your results will show your risk level and personalized recommendations.
Risk Assessment Form
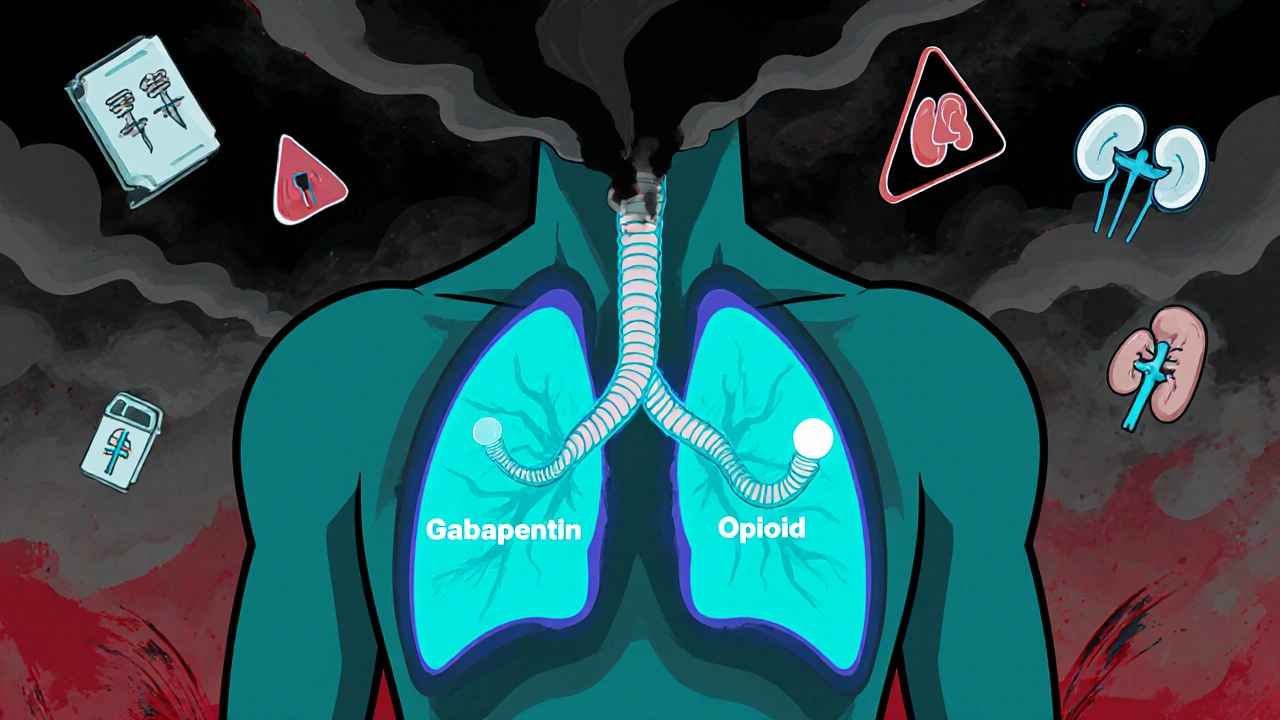
When doctors prescribe gabapentin or pregabalin for nerve pain, many assume they’re adding a safe, non-addictive option to a pain plan-especially when opioids are involved. But here’s the truth: combining these drugs doesn’t just add up. It multiplies the risk of something deadly-respiratory depression.
What Exactly Is Respiratory Depression?
Respiratory depression means your breathing slows down enough to become dangerous. Your body doesn’t get enough oxygen, carbon dioxide builds up, and your brain stops telling your lungs to work. In severe cases, it leads to coma or death. This isn’t theoretical. Between 2012 and 2017, the FDA recorded 49 cases of respiratory depression linked to gabapentinoids. Of those, 12 ended in death. Every single fatal case involved either an opioid, another CNS depressant, or an existing breathing problem.Why Gabapentinoids and Opioids Are a Dangerous Mix
Gabapentin and pregabalin were never designed to be painkillers like opioids. They work on nerve signals, not on opioid receptors. But here’s the twist: they still slow down your breathing-even on their own. A small 2016 study with healthy volunteers showed that a single dose of gabapentin caused more breathing pauses during sleep than a placebo. Pregabalin did the same. When you add opioids into the mix, the effect isn’t just added-it’s amplified. Studies like the one by Myhre et al. found that when people took both pregabalin and remifentanil (a strong opioid), their CO2 levels rose significantly higher than with either drug alone. That’s additive respiratory depression. Your brain gets confused. It’s already being told to slow breathing by the opioid. Then gabapentinoids hit, and the brakes get pressed harder. Even worse, gabapentinoids might reverse opioid tolerance. Normally, people who take opioids long-term build up a tolerance-they need higher doses to feel the same effect. But gabapentinoids can reset that tolerance, making the same opioid dose suddenly more powerful-and more dangerous.The Numbers Don’t Lie
A landmark 2017 study in PLOS Medicine looked at over 2 million patients over 16 years. It found that if you were prescribed both an opioid and a gabapentinoid, your risk of dying from an opioid-related cause jumped by 50%. For those on very high doses of gabapentin, the risk nearly doubled-up 98%. That’s not a small increase. That’s a life-or-death spike. And it’s not rare. In 2017, nearly 1 in 4 new prescriptions for pregabalin came with an opioid. Gabapentin wasn’t far behind. Why? Because doctors were trying to reduce opioid doses. They thought gabapentinoids were a safer alternative. But the data shows that instead of cutting risk, they were creating a new one.
Who’s Most at Risk?
Not everyone who takes these drugs together will have problems. But some people are far more vulnerable:- Older adults-lung function declines with age, and the brain’s response to depressants weakens.
- People with COPD, sleep apnea, or asthma-their breathing is already compromised.
- Those with kidney problems-gabapentin and pregabalin are cleared by the kidneys. If your kidneys aren’t working well, the drugs build up in your blood, increasing side effects.
- People on high doses-the higher the dose, the greater the risk. The FDA warns that doses above 300 mg of gabapentin or 150 mg of pregabalin per day raise the danger significantly.
What the Regulators Say
In April 2019, the U.S. Food and Drug Administration (FDA) issued a formal warning. All gabapentinoid labels now carry a boxed warning-the strongest type-about the risk of respiratory depression when combined with opioids. The UK’s MHRA did the same. These aren’t gentle suggestions. They’re red flags. The FDA’s review found that 92% of gabapentinoid-related respiratory depression cases involved either another CNS depressant or a pre-existing breathing issue. In other words, if you’re taking an opioid, you’re already in the danger zone.Are Gabapentinoids Even Necessary?
Here’s the uncomfortable truth: the evidence that gabapentinoids improve pain control when added to opioids is weak. A 2020 study in JAMA Network Open analyzed over 5.5 million surgical patients. It found that in most cases, gabapentinoids didn’t significantly reduce pain or opioid use after surgery. In some types of surgery, like cardiothoracic procedures, opioid-related respiratory depression hit 17% of patients-even without gabapentinoids. Adding them didn’t help. It only made things riskier. So why are they still prescribed so often? Because they’re easy. They’re not controlled substances. They don’t cause euphoria. Doctors think they’re safe. But safety isn’t just about addiction. It’s about breathing.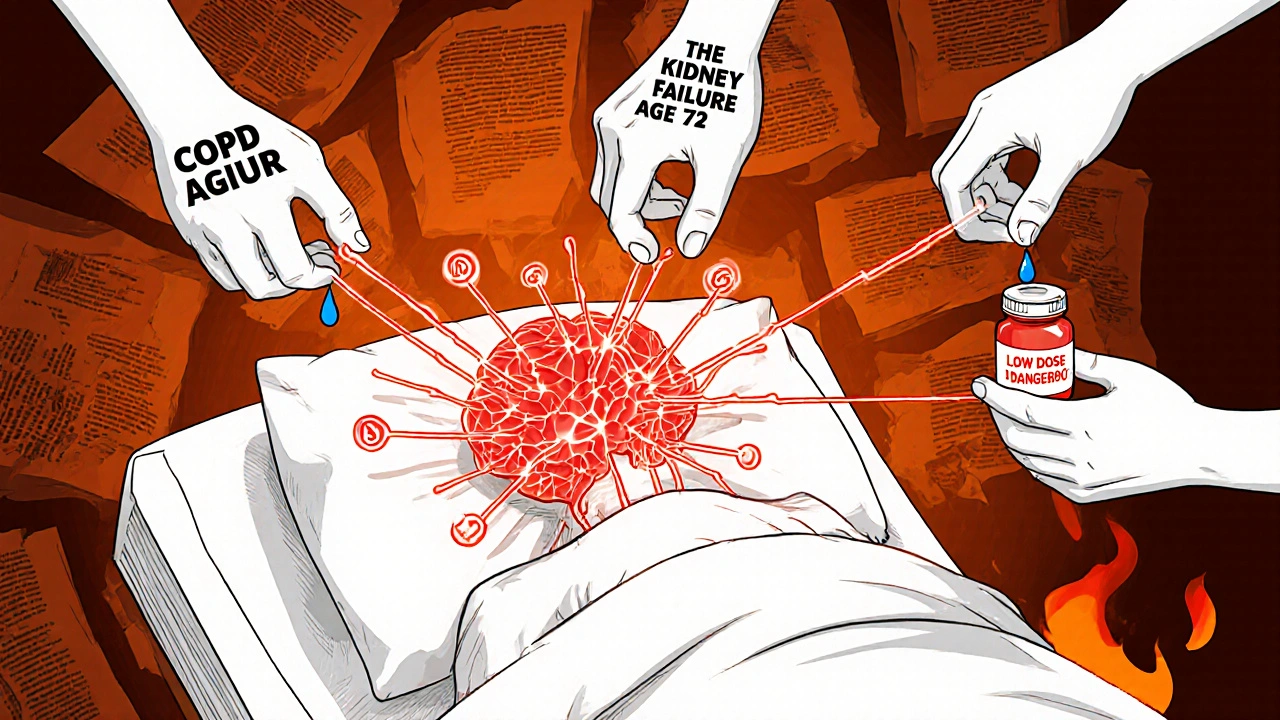
What Should You Do?
If you’re taking gabapentin or pregabalin with an opioid, don’t stop suddenly. That can cause seizures or withdrawal. But do talk to your doctor. Ask these questions:- Is this combination still necessary?
- Could I try a different pain treatment without this risk?
- What’s my kidney function? Do I need a lower dose?
- Am I on the lowest effective dose of both drugs?
Alternatives to Consider
If gabapentinoids aren’t working well and carry this risk, what else can help with nerve pain?- SNRIs like duloxetine or venlafaxine-these antidepressants are FDA-approved for neuropathic pain and don’t cause respiratory depression.
- Topical treatments like lidocaine patches or capsaicin cream-no systemic effects, no breathing risk.
- Physical therapy and nerve blocks-non-drug options that often work better than people expect.
- Cognitive behavioral therapy-helps manage chronic pain without drugs at all.
Bottom Line
Gabapentinoids aren’t harmless. When mixed with opioids, they turn a known risk into a life-threatening one. The data is clear: this combination kills. And it’s not rare. It’s happening in clinics across the country because doctors thought they were being cautious. If you’re on both, talk to your provider. Ask if the benefits still outweigh the risks. There are safer ways to manage pain. You don’t have to accept this level of danger just because it’s common.Can gabapentin or pregabalin cause breathing problems on their own?
Yes. While the risk is higher when combined with opioids, studies show gabapentin and pregabalin can cause respiratory depression even alone. A 2016 trial found that healthy volunteers had more breathing pauses during sleep after taking gabapentin compared to placebo. The FDA confirmed cases of respiratory depression with gabapentinoid monotherapy, though these are less common than when opioids are involved.
How do I know if I’m at risk for respiratory depression?
You’re at higher risk if you’re over 65, have COPD, sleep apnea, kidney disease, or are taking high doses of either drug. Being on other sedatives like benzodiazepines or alcohol also increases danger. If you’ve ever felt unusually sleepy, confused, or had trouble catching your breath while on these medications, talk to your doctor immediately.
Do all gabapentinoids carry the same risk?
Both gabapentin and pregabalin carry the same respiratory depression risk. Pregabalin is more potent and may be more likely to cause side effects at lower doses, but neither is safer than the other in this regard. The FDA’s warning applies to all gabapentinoid medications, regardless of brand or generic name.
Can I just lower my dose instead of stopping?
Reducing the dose can lower your risk, but only if done under medical supervision. Never stop gabapentinoids suddenly-they can trigger seizures. Work with your doctor to taper slowly while exploring safer alternatives. A low dose of gabapentin (under 300 mg/day) or pregabalin (under 150 mg/day) carries less risk, but still requires caution if you’re on opioids.
Why were gabapentinoids prescribed so often with opioids if the risk was known?
In the 2010s, CDC guidelines pushed doctors to reduce opioid prescribing. Gabapentinoids seemed like a safe, non-addictive alternative. Many believed they reduced opioid needs and improved pain control. But research later showed they didn’t improve outcomes significantly-and actually increased the risk of death. The problem wasn’t lack of evidence; it was delayed recognition of the interaction.
Are there any pain medications that are safer than gabapentinoids when using opioids?
Yes. SNRIs like duloxetine and venlafaxine are proven for nerve pain and don’t affect breathing. Topical treatments like lidocaine patches or capsaicin cream have no systemic effects. Physical therapy, acupuncture, and cognitive behavioral therapy also help manage chronic pain without respiratory risks. Always ask your doctor about non-depressant options before adding another CNS-slowing drug.

Hannah Machiorlete
I’ve been on gabapentin for 5 years for fibromyalgia and my doctor just added oxycodone last year because the pain got worse. I didn’t think twice until I started nodding off in the middle of the day. One time I woke up gasping for air at 3am. I didn’t tell anyone until I read this. Now I’m scared to even take my meds.
prasad gali
The pharmacokinetic synergy between GABA-B analogs and mu-opioid agonists induces dose-dependent CNS depression via GABAergic potentiation and respiratory center suppression in the medulla. This is not anecdotal-it’s neuropharmacology 101. The FDA warning was long overdue, yet prescribers still treat these as benign adjuncts. It’s institutional negligence masked as compassionate care.
Paige Basford
My mom was on both and had a near-fatal episode last winter. She didn’t even know it was the combo causing her to feel like she couldn’t breathe. She thought it was just aging. I’m so glad this got shared. I’ve been pushing her doctor to switch her to duloxetine-finally got her on it last month. She’s sleeping better, breathing better, and actually smiling again. Small wins, right?
Ankita Sinha
Wait-so gabapentin alone can cause breathing pauses? I thought it was just the opioids. I’ve been taking 900mg a day for neuropathy and I’ve been feeling foggy since last summer. Maybe I should get my levels checked. I never connected the dots. Thanks for the clarity.
william volcoff
Let’s be real: the system rewarded doctors for prescribing gabapentinoids like they were vitamins. No DEA scheduling, no paperwork, no audits. Meanwhile, the data was sitting there for years. Now we’re stuck with a generation of patients on polypharmacy cocktails because the easiest answer was the one that got paid. We didn’t need more pills-we needed better pain management infrastructure.
Freddy Lopez
There’s a deeper question here: why do we equate safety with non-addictiveness? Just because a drug doesn’t make you euphoric doesn’t mean it doesn’t kill you. We’ve built a culture that mistakes absence of pleasure for absence of danger. But breathing isn’t optional. And when we ignore that, we’re not being compassionate-we’re being careless.
Brad Samuels
I’m a nurse who’s seen this play out too many times. One patient, 72, on gabapentin and hydrocodone, stopped breathing in the hallway. We revived him. His wife said, ‘The doctor said it was fine.’ I cried after shift. We’re not protecting people-we’re just following the script. We need better training. And we need to listen when patients say, ‘I feel like I can’t catch my breath.’
Mary Follero
My cousin was on gabapentin for sciatica and oxycodone after back surgery. She ended up in the ICU with CO2 narcosis. They didn’t realize it was the combo until they pulled her meds. She’s fine now, but she’s terrified. She’s doing CBT and physical therapy instead. Honestly? She feels more in control than she ever did on pills. If you’re on both, don’t wait for a crisis. Talk to your doctor. There are other ways. And you’re not weak for asking.
Will Phillips
THEY KNEW THIS WAS A KILLER COMBO AND STILL PUSHED IT FOR PROFIT. DOCTORS AREN’T HEALERS THEY’RE PHARMACEUTICAL AGENTS. THE FDA IS A TOY OF BIG PHARMA. I’M NOT TAKING ANYTHING FROM THEM EVER AGAIN. IF YOU’RE ON GABA+OPIOID YOU’RE A LIVING EXPERIMENT. STOP. NOW. BEFORE THEY KILL YOU IN YOUR SLEEP.