Gabapentin and Opioids: Risks, Interactions, and What You Need to Know
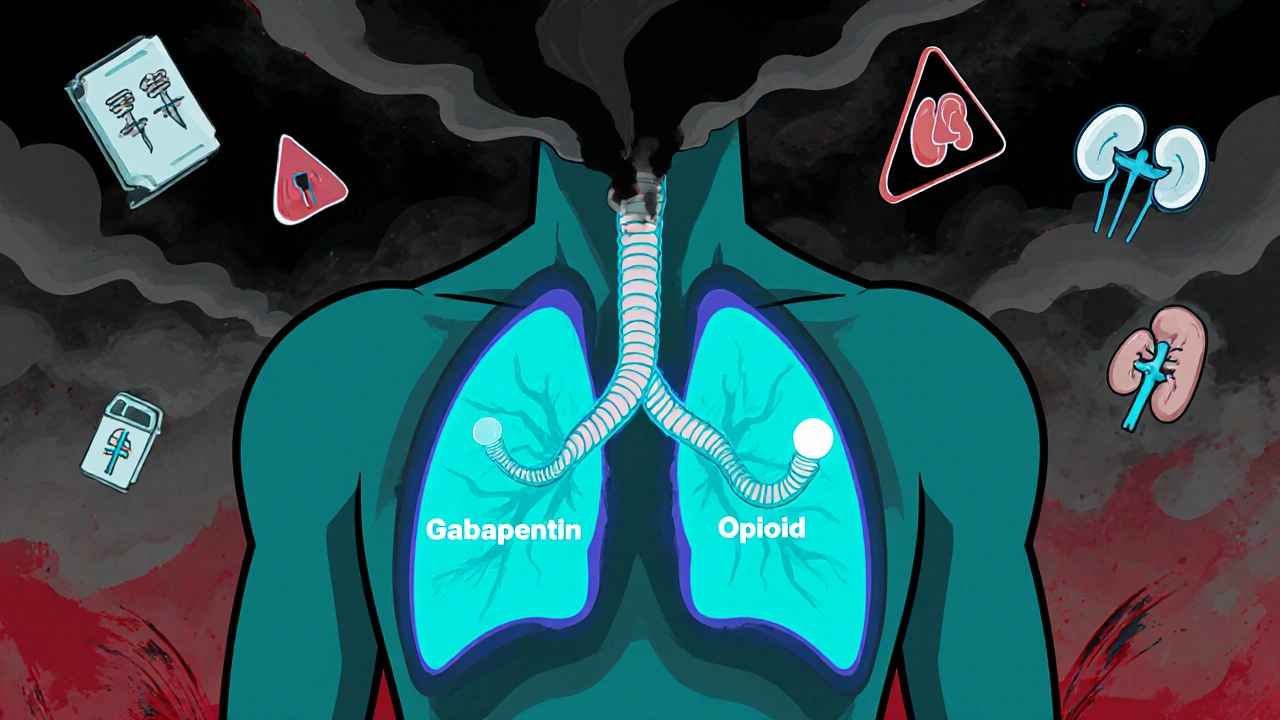
When you take gabapentin and opioids, a combination of a nerve pain medication and a powerful painkiller. Also known as anticonvulsant-opioid pairing, it’s becoming more common—especially for chronic pain—but it’s not harmless. This mix can slow your breathing to dangerous levels, even if you’re taking both exactly as prescribed. The CDC and FDA have warned about this combo because it doesn’t just add up—it multiplies risk.
Why does this happen? gabapentin, a drug originally made for seizures and nerve pain. Also known as Neurontin, it affects the brain’s electrical activity and can calm overactive nerves. opioids, like oxycodone, hydrocodone, or morphine. Also known as narcotic pain relievers, they bind to receptors in your brain and spinal cord to reduce pain signals. Together, they both depress your central nervous system. That means your breathing slows down. Your heart rate drops. Your body gets less oxygen. In some cases, this leads to coma or death—especially if you’re older, have sleep apnea, or take other sedatives like benzodiazepines.
You might think, "I’m not taking high doses," or "I’ve been on this combo for years." But studies show that even low doses of gabapentin can raise the risk of opioid overdose by 60% or more. People with chronic pain—back issues, diabetic neuropathy, fibromyalgia—are often prescribed both because doctors want to reduce opioid amounts. But instead of lowering risk, this mix can make things worse. Real patients have ended up in the ER after adding gabapentin to their pain routine, not because they abused it, but because they trusted their doctor’s advice without knowing the hidden danger.
It’s not just about overdosing. This combo also makes you drowsier, clumsier, and more likely to fall. For older adults, that’s a major concern. It can also make you feel foggy or depressed. And if you suddenly stop one of these drugs, withdrawal can be brutal—especially with gabapentin, which many don’t realize can cause seizures if quit cold turkey.
What should you do? If you’re on both, talk to your doctor. Don’t stop either on your own. Ask: "Is this combination still necessary?" "Are there safer alternatives?" "Could I try non-opioid options like physical therapy, antidepressants, or nerve blocks?" Some people find relief with gabapentin and opioids only for short periods, then switch to something less risky. Others need both—but they need monitoring, like regular breathing checks or home oxygen sensors.
Below, you’ll find real stories and science-backed guides from people who’ve lived through this. You’ll see how others spotted the warning signs, what their doctors missed, and how they found safer paths. This isn’t about fear—it’s about awareness. You deserve pain relief without putting your life at risk.
Gabapentinoids and Opioids: The Hidden Danger of Combined Respiratory Depression
Combining gabapentinoids with opioids can dangerously slow breathing-even kill. Learn why this interaction is deadlier than many doctors realize, who’s at risk, and what safer alternatives exist.
More