EHR Allergy Management: How Digital Records Help Track and Prevent Drug Reactions
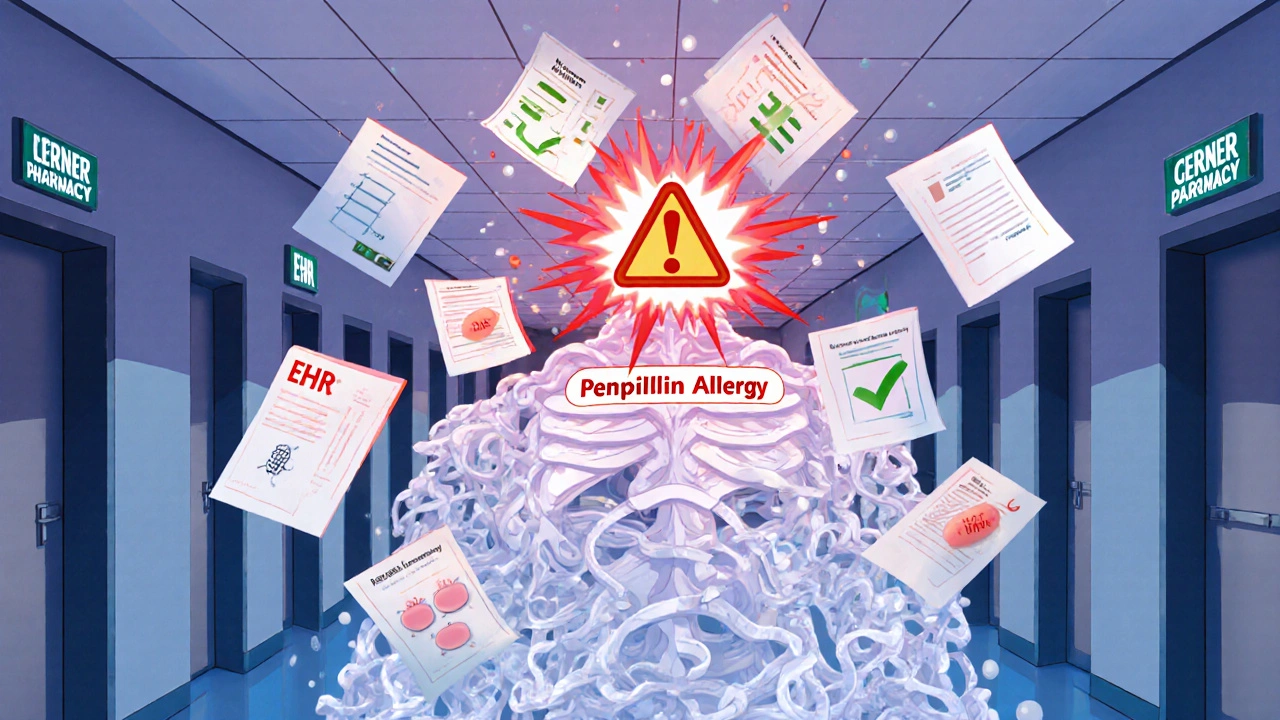
When it comes to EHR allergy management, the use of electronic health records to accurately document, flag, and act on patient drug allergies. Also known as digital allergy tracking, it’s not just about typing "penicillin allergy" into a field—it’s about preventing life-threatening mistakes before they happen. Every year, thousands of patients are harmed because their allergy history was missing, outdated, or misunderstood. EHR systems fix that by making allergies visible, actionable, and hard to ignore.
Real electronic health records, digital versions of a patient’s medical history used by clinics and hospitals. Also known as EMRs, they don’t just store data—they connect it. If a patient has a documented allergic drug reaction, a true immune response to a medication, not just a side effect. Also known as drug hypersensitivity, it to amoxicillin, the system should block any new prescription for it—even if the doctor forgets to check. It should also alert staff if the patient is given a related antibiotic like cephalexin. This isn’t science fiction. Hospitals using smart EHRs have cut allergic reaction rates by over 40%.
But EHR allergy management isn’t just about alerts. It’s about context. A patient might say they’re allergic to "sulfa," but that could mean sulfa antibiotics, sulfa diuretics, or even sulfa in some diabetes pills. Smart systems ask: Which one? When did it happen? What were the symptoms? Hives? Swelling? Trouble breathing? That detail changes everything. If a patient had a mild rash ten years ago, they might still safely take a sulfa diuretic today. But if they went into anaphylaxis, the system locks it down. That’s why many EHRs now use structured fields instead of free text. And why they link to databases like the FDA’s adverse event reports to flag newly reported reactions.
It’s also about who’s using it. Nurses entering meds. Pharmacists reviewing scripts. Even patients updating their own records through portals. When all those people are working from the same accurate data, mistakes drop. One study found that when patients could edit their own allergy lists in the EHR, 32% of them corrected errors—like listing "aspirin allergy" when they’d only had a stomach ache after taking it. That’s not an allergy. That’s a side effect. And confusing the two leads to worse care, higher costs, and unnecessary avoidance of safe drugs.
What you’ll find in the posts below are real stories and tools that show how this works in practice. From how to tell the difference between a side effect and a true allergy, to how EHRs prevent double dosing in kids, to why mislabeling reactions can cost lives. You’ll see how one patient’s penicillin label led to three unnecessary antibiotics, how a simple EHR alert stopped a deadly combo of ephedrine and MAOIs, and how probiotics might actually help reduce allergy risks over time. These aren’t theory pieces. They’re what happens when systems get smarter—and when people finally stop guessing.
How to Update Your Allergy List Across All Healthcare Providers
Learn how to fix your outdated allergy list across all healthcare providers to avoid dangerous drug reactions. Step-by-step guide to verify, update, and share your true allergy history.
More