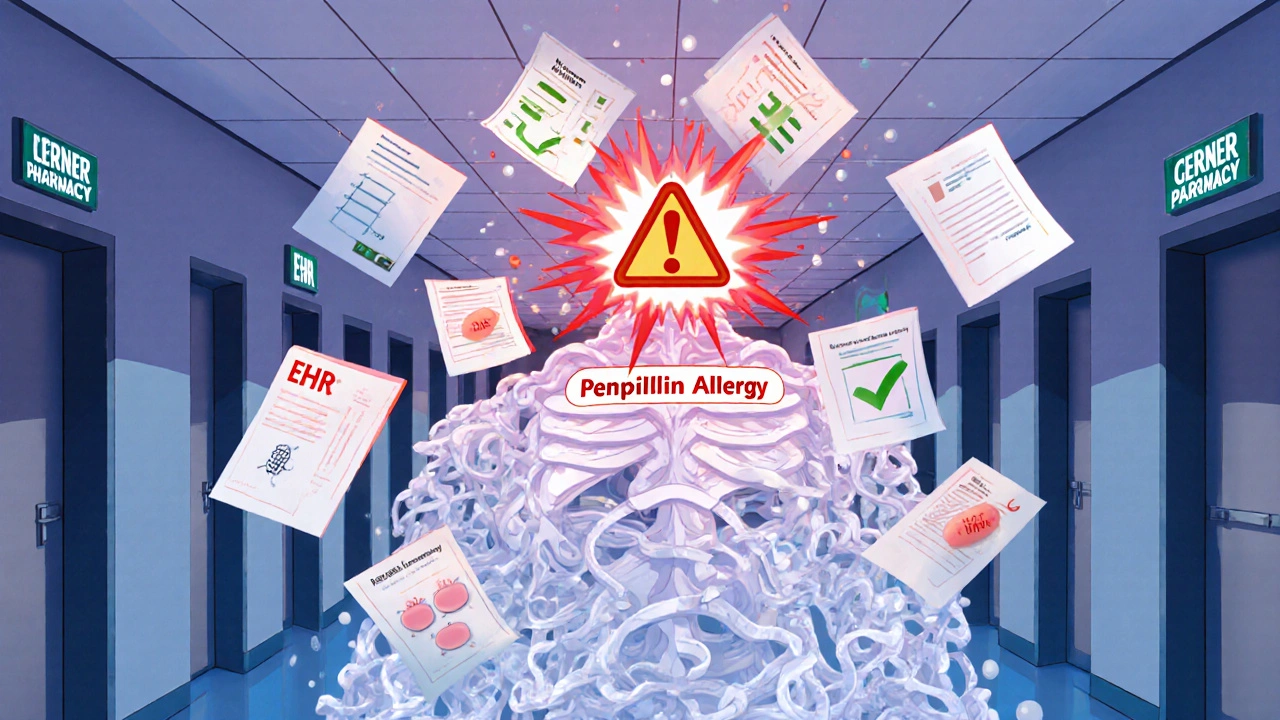
Every time you visit a new doctor, pharmacist, or emergency room, your allergy list could be wrong. And that’s not just a paperwork issue-it’s a life-or-death risk. About 5% of hospitalized patients suffer an adverse drug reaction because someone misread or missed their allergy history. For some, that means anaphylaxis. For others, it means being stuck with a more expensive, less effective antibiotic because a doctor thinks they’re allergic to penicillin-even though they haven’t had a reaction in 20 years.
The truth? Your allergy list is probably outdated. Studies show that between 7% and 12.9% of the allergies listed in electronic health records (EHRs) don’t match what patients actually experience. Some are false positives. Others are incomplete. A few are just plain wrong. And unless you take action, each new provider you see might be working with the same flawed information.
Why Your Allergy List Is So Often Wrong
It’s not your fault. The system is broken. Most doctors rely on what’s typed into the EHR system during your last visit. If you told a nurse you got a rash after amoxicillin five years ago, that’s now a permanent label-no matter if you’ve taken it since without issue. Even worse, many providers don’t verify. They just copy-paste.
Here’s how it goes wrong:
- You say, “I’m allergic to penicillin.” The provider writes “Penicillin allergy-rash.”
- No one asks if you’ve taken it since. No one checks your pharmacy records. No one tests it.
- Next time you’re sick, you get a different antibiotic-maybe one that costs $300 instead of $10.
- Years later, another doctor sees “Penicillin allergy” and avoids it entirely-even if you’ve taken it safely 10 times.
And it’s not just drugs. Food allergies, environmental triggers, and even reactions to latex or contrast dye often get lumped into the same messy list without clear details. That’s why the U.S. government mandated new rules in January 2025: every certified EHR system must now store allergies with specific details-like severity, timing, and whether it’s been verified by testing.
What Your Allergy List Should Actually Include
Under the 2025 ONC standards, your allergy record isn’t just a name. It needs four key pieces of information:
- What you’re allergic to-Use the exact term: “Amoxicillin,” not just “antibiotic.”
- What happened-“Hives,” “swelling,” “trouble breathing,” or “nausea.” Don’t say “bad reaction.”
- When it happened-“2019,” “after first dose,” “2 hours after taking.”
- Verification status-Was it confirmed by a test? Is it patient-reported? Is it unverified?
Why does this matter? Because “penicillin allergy” is the most overreported allergy in the U.S. Up to 90% of people who think they’re allergic to penicillin aren’t. A simple skin test or oral challenge can prove it. But if your record just says “penicillin allergy” with no details, no doctor will risk testing you.
How to Update Your Allergy List Yourself
You’re the only one who knows your body. No EHR system will fix this for you unless you step in. Here’s how to take control:
1. Gather All Your Records
Log into every patient portal you have-your primary care doctor, specialists, hospital systems, even the pharmacy you use. Download your allergy list from each one. Don’t assume they’re the same. Compare them side by side. You’ll likely find differences.
2. Identify the Inaccuracies
Ask yourself:
- Did I ever have a true allergic reaction-or just a side effect?
- Have I taken this drug since the reaction? Did I have issues?
- Was this allergy diagnosed by a doctor-or just assumed?
For example: If you broke out in hives after a single dose of amoxicillin as a child but have taken it since without issue, that’s not an active allergy. It’s a past event that was never re-evaluated.
3. Request a Formal Allergy Review
Make an appointment with your primary care doctor or an allergist. Say: “I’d like to review my allergy list. I think some of these might be outdated.” Bring your compiled records. Ask if you should get tested for any allergies you’re unsure about.
Penicillin testing is safe, quick, and covered by most insurance. It involves a skin prick and, if negative, a small oral dose under supervision. Results are ready in under an hour. If the test is negative, your doctor can remove the allergy label from your record.
4. Update Every System
Once your allergy list is corrected:
- Log into each patient portal and edit your allergy list manually.
- Call each provider’s records department and ask them to update your file.
- Ask your doctor to send a summary to any specialists you see.
Don’t rely on one system to update the others. Each EHR operates independently. Epic, Cerner, and others don’t automatically sync allergy changes unless they’re part of a network with advanced reconciliation tools.
What Your Doctor Should Be Doing (But Often Isn’t)
Good providers use tools like NLP-powered reconciliation systems that scan your clinical notes, lab results, and medication history to flag mismatches. For example, if your chart says “penicillin allergy” but you’ve been prescribed and taken amoxicillin five times in the last two years, the system should alert the doctor.
But only 40% of U.S. healthcare systems have these advanced tools. Most still rely on manual checks. That’s why you can’t wait for your doctor to catch it-you have to lead the process.
Ask your provider: “Do you use a system that checks for conflicting allergy information across my records?” If they say no, ask them to manually review your list at every visit.
What to Do If You’re in an Emergency
Emergency rooms don’t have time to check your portal. That’s why you need a physical backup.
- Keep a printed copy of your current, verified allergy list in your wallet or phone case.
- Use a medical ID bracelet if you have severe allergies (anaphylaxis to nuts, bee stings, etc.).
- Save a screenshot of your updated allergy list in your phone’s photos folder with the title: “My Current Allergies - Updated [Date].”
In a crisis, paramedics and ER staff will look for these. Don’t assume they’ll find your digital record.
The Bigger Picture: Why This Matters Beyond You
Inaccurate allergy records cost the U.S. healthcare system over $1.2 billion a year. Why? Because doctors avoid safe, cheap drugs and use broader-spectrum antibiotics instead. That leads to more side effects, longer hospital stays, and rising antibiotic resistance.
When you fix your allergy list, you’re not just protecting yourself. You’re helping reduce unnecessary drug use for everyone. A 2022 study showed that when hospitals implemented proper allergy reconciliation, inappropriate antibiotic prescriptions dropped by 23.6%.
And it’s getting easier. By 2026, Medicare will tie 2.3% of hospital payments to accurate allergy documentation. That means hospitals are finally being forced to fix their systems. But until then, the burden is on you.
What’s Next? Your Action Plan
Here’s your simple, 5-step plan to get your allergy list right-for good:
- Collect-Download your allergy list from every provider and pharmacy portal.
- Compare-Look for duplicates, inconsistencies, or vague entries.
- Verify-Schedule a visit with your doctor or allergist to review and test if needed.
- Update-Edit your records in every system you use.
- Share-Print a copy. Save a digital version. Tell your family.
Do this once a year. Or anytime you start a new medication, see a new specialist, or have a new reaction. It takes less than an hour. And it could save your life.
Can I remove an allergy from my record without testing?
It depends. If your allergy was never confirmed by testing and you’ve taken the drug safely since, your doctor can remove it based on your history. But for high-risk allergies like anaphylaxis, testing is strongly recommended before removal. Never remove an allergy label on your own-always work with a provider.
Why do different doctors have different allergy lists?
Because most EHR systems don’t automatically share or reconcile allergy data. One doctor may copy your list from a previous visit, while another types it in manually from memory. Without a centralized, standardized system, inconsistencies are common. That’s why you need to check and update your list yourself.
Are food allergies included in EHR allergy lists?
Yes, but they’re often poorly documented. Only about 32.6% of EHRs accurately capture food or environmental allergies with enough detail to be useful. Many providers only record drug allergies. If you have a food allergy, make sure it’s listed clearly with symptoms and timing-and confirm it’s in every system you use.
How long does it take to update my allergy list across all providers?
It can take a few weeks. Each provider has its own process for updating records. Some allow instant edits through patient portals. Others require a written request or a doctor’s note. Start with your primary care provider-they can help coordinate updates with specialists. Don’t wait for perfection; update one system at a time.
What if I don’t have access to a patient portal?
Call the medical records department at each provider’s office. Ask for a copy of your allergy list and request updates in writing. You have the legal right to access and correct your health records under HIPAA. Send your request by certified mail if needed, and keep a copy for your records.

Iives Perl
They're tracking your allergies but not your meds? LOL. Next they'll say 'we can't find your heartbeat in the system.' 😏
Cecily Bogsprocket
I used to think my penicillin allergy was just a childhood scare-until I had a rash after a random dose at 28. Turns out, it was a viral infection. But no one ever asked. I’m glad this post exists. Taking control of your health isn’t selfish-it’s survival. You’re not being difficult. You’re being smart.
steve stofelano, jr.
It is imperative to underscore the significance of standardized allergy documentation within electronic health records. The absence of granular data-such as severity, temporal context, and verification status-constitutes a systemic failure in patient safety infrastructure. The 2025 ONC mandate represents a necessary, albeit overdue, corrective measure in clinical informatics.
Savakrit Singh
📊 1.2B USD lost annually? 📉 90% of penicillin 'allergies' are false? 🤯 This isn’t just bad record-keeping-it’s a public health disaster. And guess who pays? The patient. The system. The planet. We need AI-driven reconciliation NOW. Not in 2026. NOW. 🚨 #HealthcareIsBroken
Jebari Lewis
I’ve spent 14 months chasing my allergy records across 7 providers. Every time I update one, another reverts. I called the EHR vendor. They said ‘it’s not our problem.’ I have screenshots of my corrected list in my phone, my wallet, and my fridge. This isn’t healthcare. It’s a bureaucratic obstacle course. If you’re reading this: DO NOT WAIT. START TODAY. You’re your only advocate.
Emma louise
Oh wow, so now we’re supposed to be our own medical clerks? Next they’ll ask us to fix the X-ray machines too. I mean, if the government can’t get a database right, why should I care? 🤷♀️
sharicka holloway
I used to think I was overreacting when I asked my doctor to double-check my list. Now I know I was just being responsible. I showed my mom how to do this last week. She’s 72 and never had a patient portal. We printed it out, sat at the kitchen table, and called her cardiologist together. She cried. Not because she was scared-because someone finally listened.
Alex Hess
Wow. Another ‘you’re responsible for fixing broken systems’ guilt trip. This is what happens when you let patients manage their own medical records. Next you’ll tell us to code our own EHRs. The system is broken? Fix it. Don’t dump the labor on the patient.
Leo Adi
In India, we don’t even have digital records in most clinics. My cousin’s allergy was written on a sticky note taped to his file. He got the wrong drug. He survived. But I think about it every time I see a doctor here. Maybe the solution isn’t tech-it’s culture. We need to teach people to speak up. Even if their voice shakes.
Melania Rubio Moreno
why do all the docs just copy paste?? like i had a rash from ibuprofen in 2015 and now its on every record as 'anaphylaxis to NSAIDs'... i mean... come onnnnn
Gaurav Sharma
Let me be clear: This is not a patient issue. It is a corporate failure. EHR vendors profit from fragmentation. They design systems that don’t talk to each other. Then they charge hospitals extra to ‘integrate.’ The real villain isn’t the patient who forgets to update their portal-it’s the $20B industry that built the broken machine.
Jonah Thunderbolt
My mother died because they gave her a drug she was ‘allergic’ to-according to a 2003 note she never even told them about. She had dementia. She didn’t remember. They didn’t check. They didn’t care. Now I carry her updated list in my phone. I print it. I wear a bracelet. And every time I see a new doctor, I say: ‘I’m not here to argue. I’m here to survive.’ And I don’t care if they roll their eyes. I’ve lost too much to care.