Psychiatric Medication Interaction Checker
Check Medication Combinations
Select your current medications to see potential dangerous interactions. Based on Australian hospital data showing 47% of psychiatric adverse events come from drug interactions.
DANGER: SERIOUS INTERACTION RISK
Combining these medications can cause serotonin syndrome or other life-threatening reactions.
- Confusion
- Rapid heartbeat
- Muscle rigidity
- High fever
- Seizures
Avoid this combination. Immediate medical attention required if symptoms occur.
WARNING: MODERATE INTERACTION RISK
This combination may increase side effects or reduce effectiveness. Consult your doctor before taking together.
Possible effects: Increased bleeding risk, reduced medication effectiveness, or excessive drowsiness
SAFE: NO SIGNIFICANT INTERACTION
This combination is generally safe when used together. However, always monitor for unusual side effects.
Still check with your doctor before combining any new medications.
Critical Safety Information
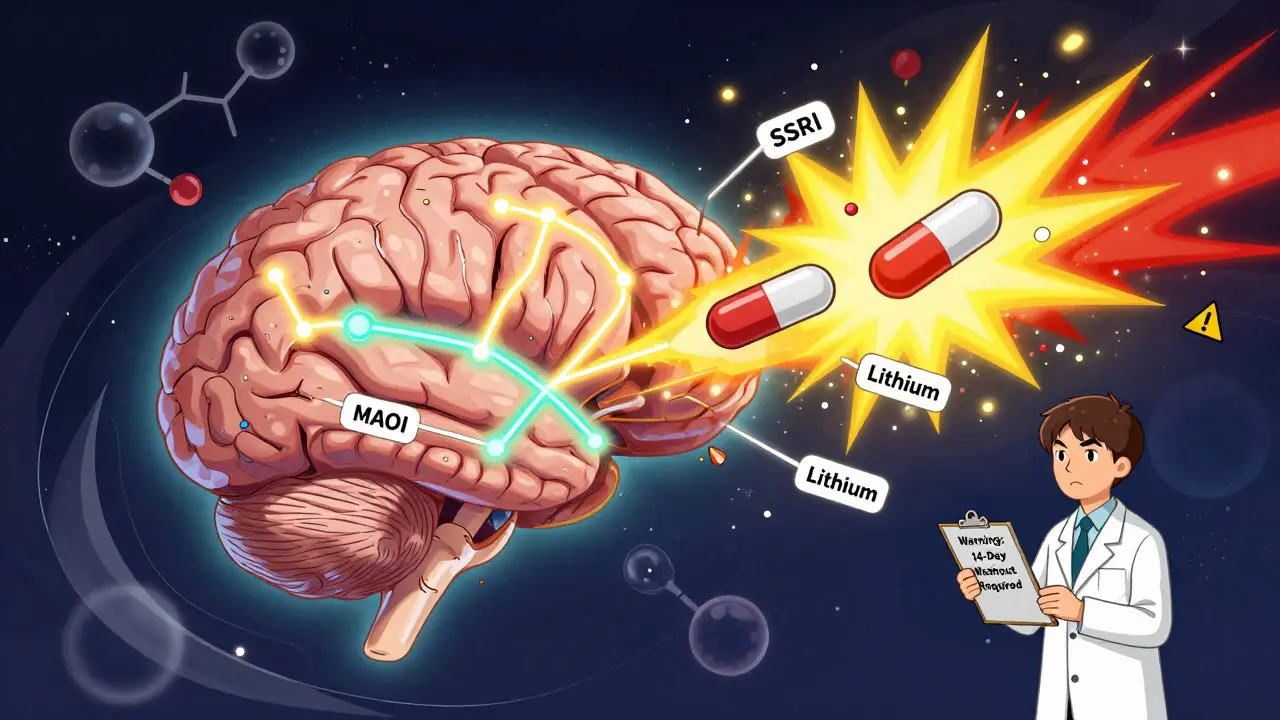
- Never skip washout periods: Wait at least 14 days between SSRI and MAOI. For fluoxetine, wait 5-6 weeks.
- Lithium warning: NSAIDs like ibuprofen can increase lithium levels by 25-50%. Use acetaminophen instead for pain relief.
- Alcohol risk: Combined with TCAs or antipsychotics, can cause dangerous breathing problems and low blood pressure.
- St. John's Wort: Can cause serotonin syndrome when combined with SSRIs, SNRIs, or MAOIs.
When you're managing mental health with medication, it's easy to focus on one pill at a time. But what happens when you add another? Or when a cold medicine, painkiller, or even a supplement enters the mix? The truth is, psychiatric medications don't work in isolation. They interact - sometimes harmfully - with other drugs, and those interactions can be life-threatening. This isn't theoretical. In Australian hospitals, nearly half of all adverse drug events in psychiatric care come from unexpected combinations. You need to know which ones to avoid.
Why These Interactions Matter
Psychiatric medications affect your brain’s chemistry. They change levels of serotonin, norepinephrine, and dopamine. That’s how they help with depression, anxiety, psychosis, and bipolar disorder. But when two drugs hit the same system, they can overdo it. Or they might block each other. Or worse - they might trigger a reaction your body can’t handle. Take serotonin, for example. Many antidepressants boost it. So do some pain meds, migraine treatments, and even herbal supplements like St. John’s Wort. If you take two of these together, serotonin can flood your system. That’s not a good thing. It can lead to serotonin syndrome - a condition with symptoms like confusion, rapid heartbeat, muscle rigidity, high fever, and seizures. In severe cases, it kills. Studies show 2% to 12% of people with serious serotonin syndrome don’t survive. The biggest danger? Starting a new medication. The first few days are the riskiest. Your body hasn’t adjusted. Your doctor might not know everything you’re taking. And if you’re on multiple prescriptions, the chance of a bad combo goes up fast.High-Risk Drug Classes
Not all psychiatric drugs are equal when it comes to interactions. Some are safer. Others? Not so much.- MAO inhibitors (MAOIs) like phenelzine (Nardil) and tranylcypromine (Parnate) are the most dangerous. They block enzymes that break down neurotransmitters. Combine them with SSRIs, SNRIs, or even certain cough syrups, and you’re playing Russian roulette with serotonin. You need a full 14-day washout period before switching to or from an MAOI. No exceptions.
- SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) are common. But not all SSRIs are the same. Fluoxetine and fluvoxamine are strong inhibitors of liver enzymes (CYP450), which means they slow down how your body processes other drugs. This can cause toxic buildup. Sertraline and citalopram? Lower risk. That’s why many doctors pick them when someone’s already on other meds.
- SNRIs like venlafaxine (Effexor) and duloxetine (Cymbalta) affect both serotonin and norepinephrine. They’re less likely to interfere with liver enzymes than SSRIs, but they still raise serotonin levels. That means they can still trigger serotonin syndrome if paired with the wrong drug.
- TCAs - tricyclic antidepressants like amitriptyline - are older. They’re effective, but they have strong anticholinergic effects. That means they dry you out, slow your heart, and make you drowsy. Combine them with antihistamines (like diphenhydramine in Benadryl), antipsychotics, or alcohol, and you’re asking for confusion, low blood pressure, or even heart rhythm problems.
- Atypical antipsychotics like quetiapine (Seroquel) and risperidone (Risperdal) vary. Quetiapine has fewer interactions. Others, especially when combined with drugs that affect liver enzymes, can cause dangerous spikes in blood levels. Lithium is especially risky when paired with these - it can push levels into toxic range.
- Lithium is a classic. It’s used for bipolar disorder. But its therapeutic window is tiny: 0.6 to 1.0 mmol/L. Too little? No effect. Too much? Seizures, kidney damage, coma. NSAIDs like ibuprofen or naproxen can increase lithium levels by 25% to 50%. Even a common cold medicine with a decongestant can mess with your sodium balance and make lithium more dangerous.
Real-World Danger Zones
Here are the combinations you need to avoid - and why.- SSRI + MAOI: This is the textbook example of a deadly combo. Serotonin skyrockets. Symptoms can start in hours. If you’ve been on an SSRI, wait at least 5 weeks before starting an MAOI. For fluoxetine, wait 6 weeks - it sticks around longer.
- SSRI/SNRI + Tramadol or Meperidine: These painkillers also raise serotonin. Tramadol, especially, has been linked to multiple serotonin syndrome deaths. Even if you’re on a low dose of an SSRI, adding tramadol isn’t worth the risk.
- Lithium + NSAIDs or Diuretics: Ibuprofen, naproxen, or hydrochlorothiazide can all spike lithium levels. If you’re on lithium and need pain relief, acetaminophen (paracetamol) is safer. Always check with your doctor before taking any new OTC medicine.
- TCAs + Alcohol: This combo doesn’t just make you sleepy. It depresses your breathing and heart rate. People have died from this mix. If you’re on a TCA, skip the wine, beer, or spirits.
- Antipsychotics + Antihistamines: Diphenhydramine (Benadryl), hydroxyzine, or even some sleep aids can add to the anticholinergic load. That means dry mouth, constipation, blurred vision - and worse, urinary retention or heart rhythm issues.
What Your Doctor Should Be Checking
Good psychiatric care doesn’t just mean prescribing a pill. It means knowing what else you’re taking. Every time you start a new medication - even something as simple as a statin or a beta-blocker - your doctor should check for interactions. They should use tools like the Quick Reference to Psychotropic Medications or drug interaction databases. They should know your full list: prescriptions, supplements, herbal products, and even recreational substances. They should also monitor you. That means:- Checking lithium levels before and after starting a new drug
- Monitoring INR if you’re on warfarin and an SSRI (levels can jump 20-30%)
- Running liver tests every 3 months if you’re on valproate or certain antipsychotics
- Doing weekly blood counts for the first 6 months if you’re on clozapine
- Using scales like PHQ-9, GAD-7, or AIMS to track both symptoms and side effects

What You Can Do
You’re not powerless here. You have a role.- Keep a complete list: Write down every medication, supplement, and herb you take. Include dosages and why you take them. Update it every time something changes.
- Ask before you take anything new: Even if it’s OTC. Even if it’s “natural.” Say: “I’m on [medication]. Is this safe to take with it?”
- Know your warning signs: If you feel agitated, confused, sweaty, shaky, or your muscles lock up after starting a new drug - get help immediately. Don’t wait. Call your doctor or go to the ER.
- Use one pharmacy: It sounds simple, but it helps. Your pharmacist can flag dangerous combos before you even leave the counter.
- Consider genetic testing: Tests for CYP2D6 and CYP2C19 enzymes can show how your body processes certain drugs. If you’ve had bad reactions before, it’s worth asking about.
The Future: Safer Prescribing
We’re getting better at this. Digital tools now alert doctors in real time when a dangerous combo is prescribed. Studies show a 37% drop in serious events when these systems are used properly. The National Institute of Mental Health is testing AI models that predict your personal risk based on your genetics, age, kidney function, and current meds. In the next few years, this could become standard. But right now? The responsibility still falls on you and your care team. No algorithm replaces a conversation. No app replaces knowing your own body. If you’re on psychiatric medication, don’t assume it’s safe. Don’t assume your doctor knows everything. Ask. Double-check. Speak up.Can I take over-the-counter painkillers if I’m on an SSRI?
It depends. Acetaminophen (paracetamol) is generally safe. Avoid NSAIDs like ibuprofen or naproxen - they can raise the risk of bleeding and interfere with how your body clears the SSRI. Always check with your doctor or pharmacist before taking any OTC painkiller.
How long should I wait between stopping an SSRI and starting an MAOI?
For most SSRIs, wait at least 14 days. But for fluoxetine (Prozac), which stays in your system longer, wait 5 to 6 weeks. Never skip this waiting period. The risk of serotonin syndrome is too high.
Is it safe to drink alcohol while on psychiatric medication?
It’s rarely safe. Alcohol can worsen drowsiness, dizziness, and low blood pressure. With TCAs or antipsychotics, it can cause dangerous breathing problems. With MAOIs, it can trigger a hypertensive crisis. Even with SSRIs, alcohol can make depression worse. Best to avoid it unless your doctor says otherwise.
What should I do if I think I’m having serotonin syndrome?
Seek emergency help immediately. Symptoms include high fever, rapid heartbeat, muscle rigidity, confusion, seizures, or loss of consciousness. Don’t wait. Call an ambulance or go to the nearest emergency room. Tell them you’re on psychiatric medication and suspect serotonin syndrome.
Can herbal supplements like St. John’s Wort interact with antidepressants?
Yes - and dangerously so. St. John’s Wort increases serotonin and can trigger serotonin syndrome when taken with SSRIs, SNRIs, or MAOIs. It can also interfere with birth control, blood thinners, and heart medications. Never take it without discussing it with your prescriber.

Write a comment