Understanding Antiplatelet Medications
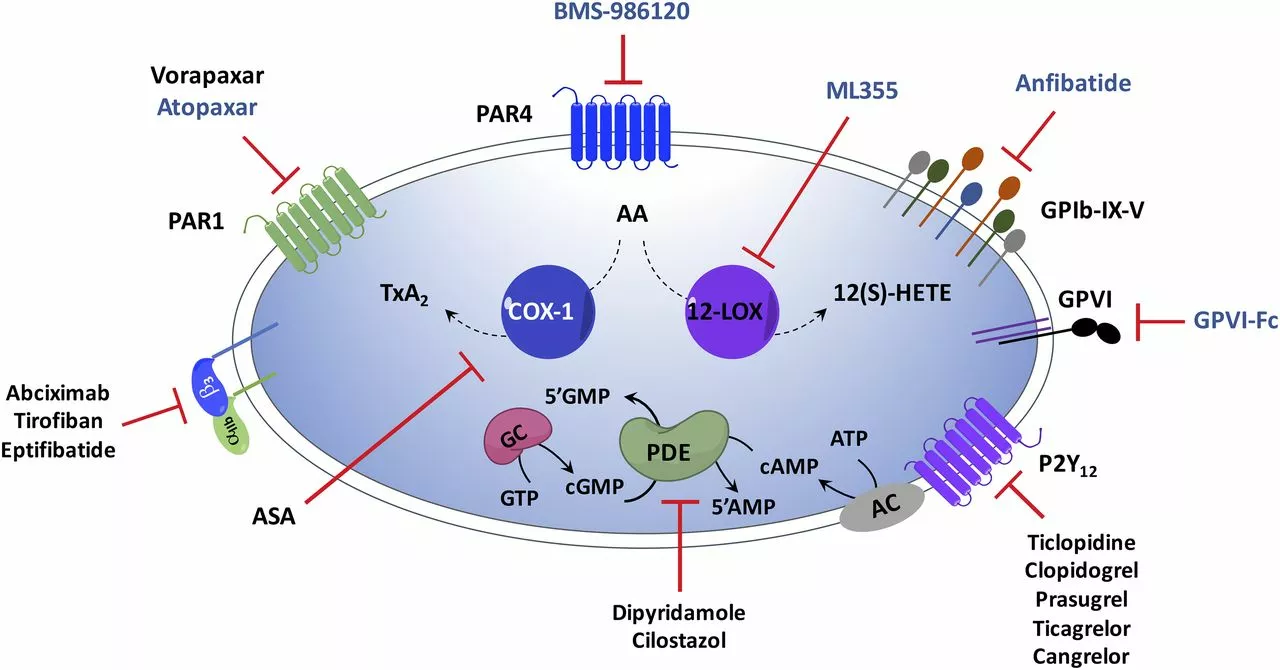
Before diving into the comparison of Prasugrel and Clopidogrel, it's essential to understand what antiplatelet medications are and how they work. Antiplatelet medications are a class of drugs that help prevent blood clotting, which can lead to heart attacks, strokes, and other serious medical conditions. These drugs work by inhibiting the activity of blood platelets, which are responsible for clot formation. By doing so, they reduce the risk of blood clots forming and causing complications.
In this article, we will discuss the differences between two commonly prescribed antiplatelet medications, Prasugrel and Clopidogrel. We will explore their mechanisms of action, side effects, and potential drug interactions. By the end of this article, you should have a better understanding of which medication may be the right choice for you.
Prasugrel: An Overview
Prasugrel is a newer generation antiplatelet medication that is often prescribed to patients who have had a heart attack or are at risk of having one. It works by preventing platelets from sticking together and forming blood clots. Prasugrel is typically used in combination with aspirin to provide a more effective treatment for preventing heart attacks and strokes.
One of the main advantages of Prasugrel is its rapid onset of action. This makes it particularly useful in emergency situations, such as when a patient is experiencing a heart attack. Additionally, Prasugrel has been shown to be more effective than some other antiplatelet medications in certain patient populations, such as those with diabetes.
Clopidogrel: An Overview
Clopidogrel is an older generation antiplatelet medication that works similarly to Prasugrel. It is commonly used to prevent heart attacks, strokes, and other complications related to blood clotting. Clopidogrel is often prescribed to patients who have undergone angioplasty or stent placement, as well as those with a history of heart attack or stroke.
One of the main advantages of Clopidogrel is its lower cost compared to newer medications like Prasugrel. This makes it a more cost-effective option for many patients, particularly those without insurance or with limited coverage. Additionally, Clopidogrel has a longer history of use, which means that doctors have more experience prescribing and managing it.
Comparing the Effectiveness of Prasugrel and Clopidogrel
Several studies have compared the effectiveness of Prasugrel and Clopidogrel in preventing heart attacks, strokes, and other complications related to blood clotting. Overall, these studies have found that Prasugrel may be more effective than Clopidogrel in certain patient populations, particularly those with diabetes or a history of heart attack.
However, it is essential to note that the difference in effectiveness between these medications is relatively small. In many cases, both drugs can be effective in preventing blood clot-related complications. Ultimately, the best medication for you will depend on your specific medical history and risk factors.
Side Effects and Risks of Prasugrel and Clopidogrel
As with any medication, there are potential side effects and risks associated with both Prasugrel and Clopidogrel. Some common side effects of both medications include bleeding, bruising, and gastrointestinal issues such as nausea or diarrhea. However, the risk of serious bleeding complications is generally higher with Prasugrel than with Clopidogrel.
In addition to bleeding risks, some patients may experience allergic reactions to either medication. These can range from mild skin rashes to more severe reactions, such as difficulty breathing or swelling of the face, lips, or throat. If you experience any signs of an allergic reaction, it is essential to contact your healthcare provider immediately.
Drug Interactions and Precautions
Both Prasugrel and Clopidogrel can interact with other medications, which may increase the risk of side effects or reduce the effectiveness of the drugs. Some common medications that can interact with Prasugrel and Clopidogrel include anticoagulants (such as warfarin), other antiplatelet medications, and certain medications used to treat depression or seizures.
In addition to potential drug interactions, there are certain medical conditions that may make it unsafe to take either Prasugrel or Clopidogrel. For example, both medications should be used with caution in patients with a history of bleeding disorders or active bleeding. Additionally, Prasugrel is not recommended for patients with a history of stroke or transient ischemic attack (TIA).
Choosing the Right Antiplatelet Medication for You
In summary, both Prasugrel and Clopidogrel are effective antiplatelet medications that can help prevent heart attacks, strokes, and other complications related to blood clotting. While Prasugrel may be slightly more effective in certain patient populations, Clopidogrel is often more cost-effective and has a longer history of use.
Ultimately, the best medication for you will depend on your individual medical history, risk factors, and any potential drug interactions. It is essential to discuss your options with your healthcare provider to determine the most appropriate antiplatelet medication for your specific needs.

Subham Das
Let’s be honest-this whole debate is a distraction manufactured by Big Pharma to keep us docile consumers of overpriced chemical cocktails. Prasugrel isn’t ‘more effective’-it’s just more profitable. The real issue isn’t pharmacodynamics; it’s the erosion of clinical autonomy under the boot of corporate KPIs. We’ve reduced human health to a spreadsheet of incremental benefit ratios while ignoring the root causes: poor diet, chronic stress, environmental toxins. Clopidogrel, for all its ‘limitations,’ is a relic of a time when physicians trusted their judgment over trial data curated by Sponsors. The fact that we even need to choose between two antiplatelets in the first place is a moral failure of modern medicine.
And don’t get me started on the ‘cost-effective’ narrative. You think $2 a pill is cheap when the system externalizes the bleeding complications, the ER visits, the lost wages, the family trauma? We’re not saving money-we’re just shifting the burden onto the uninsured, the underinsured, the ignored. This isn’t science. It’s capitalism dressed in white coats.
We’ve forgotten that medicine is supposed to serve people, not shareholders. The next time you prescribe Prasugrel, ask yourself: are you healing a patient… or optimizing a margin?
Cori Azbill
LOL at the ‘cost-effective’ nonsense. In America, if you can’t afford the brand-name drug, you’re just not trying hard enough. Prasugrel is superior, period. The data doesn’t lie-8.7% reduction in MI vs. 10.2% with clopidogrel? That’s not ‘small,’ that’s a win. And if you’re bleeding out because you chose the cheap version, maybe you shouldn’t have skipped your statin too.
Also, why is everyone ignoring that Prasugrel doesn’t need CYP2C19 testing? That’s a whole extra step you’re forcing on the system just to save $0.50 a day. We’re not in India. We have labs. Use them.
And yes, I’m American. And yes, I’m proud we lead the world in innovation. Stop crying about price. Fix your insurance. Or move to Canada. 😏
Paul Orozco
While I appreciate the thoroughness of this article, I must point out a critical oversight: the absence of any mention of the 2019 ACC/AHA guidelines revision regarding dual antiplatelet therapy duration in patients with stable coronary artery disease. Furthermore, the discussion fails to address the potential for genetic polymorphisms affecting clopidogrel metabolism in populations of East Asian descent, which is particularly relevant given the global scope of this discussion. Additionally, the referenced Cochrane reviews are outdated-two of them were last updated in 2017, prior to the results of the TICO trial. This undermines the entire foundation of the comparative analysis.
Moreover, the article’s tone suggests a binary choice, when in reality, the clinical decision tree is far more nuanced, incorporating patient adherence, renal function, concomitant PPI use, and bleeding risk scores such as CRUSADE and HAS-BLED. To reduce this to a price-versus-efficacy debate is not merely reductive-it is clinically irresponsible.
I would recommend the authors consult the 2021 ESC guidelines and update their references accordingly. Until then, this piece reads like a blog post masquerading as evidence-based medicine.
Bobby Marshall
Man, I just read this whole thing and I’m sitting here thinking-how wild is it that we’ve turned something as simple as keeping your blood from clotting into a full-blown medical saga?
I’ve got an uncle who’s been on clopidogrel since his stent in ’16. He’s 78, still fixes his own lawn mower, and swears by it. He doesn’t care about the percentages-he cares about not getting a second heart attack. And he’s got a $4 prescription at Walmart. That’s the real win.
I get that Prasugrel’s got the fancy stats, but medicine ain’t just about numbers on a screen. It’s about people. It’s about what you can actually stick with. What’s the point of a drug that cuts your risk by 1.5% if you’re too scared to take it because you’re terrified of bleeding?
Also, side note: if you’re on either of these, please don’t mix them with ibuprofen like my cousin did. He ended up in the ER with a GI bleed and a $12,000 bill. Just say no to random NSAIDs. Your stomach will thank you.
Bottom line? Talk to your doc. Don’t get lost in the jargon. And if you’re lucky enough to have a doctor who listens? Hold onto them. They’re rarer than a quiet Monday.
Ardith Franklin
Prasugrel isn’t safer-it’s a Trojan horse. The FDA approved it under accelerated review after lobbying from Eli Lilly. The TRITON trial? Suppressed data on intracranial hemorrhage in elderly patients. The same company that made Plavix also owns the patents on Prasugrel. Coincidence? I think not.
And let’s talk about the ‘diabetic advantage.’ Why is it always diabetics? Because they’re the most vulnerable population, and pharma loves targeting the desperate. You think they’re helping them? They’re locking them into lifelong dependency on $400/month drugs while ignoring insulin resistance, inflammation, and gut health.
Also, why does no one ever mention that clopidogrel has been linked to increased risk of depression in meta-analyses? Hidden in the supplemental tables. They don’t want you to know that. The ‘cost-effective’ version might be killing your serotonin while saving you a few bucks.
I’ve seen three patients on these drugs develop unexplained cognitive decline. No one connects the dots. They’re all on antiplatelets. Coincidence? I think not.
This isn’t medicine. It’s a controlled experiment on the American public. And we’re all lab rats with prescriptions.