Metformin Safety Risk Checker
Risk Assessment Tool
Based on FDA guidelines and clinical research, this tool helps you understand your personal risk factors for lactic acidosis while taking metformin.
Metformin is the most prescribed diabetes medication in the world. Over 150 million prescriptions are filled each year in the U.S. alone. It works. It’s cheap. And for most people, it’s safe. But if you’ve just started taking it, you might be dealing with stomach cramps, diarrhea, or nausea. And if you’ve heard rumors about lactic acidosis, you’re probably wondering: is this drug actually dangerous?
Why Your Stomach Hurts After Starting Metformin
More than 1 in 4 people who take metformin get gastrointestinal side effects. That’s not rare. It’s normal. The most common complaints? Diarrhea (over half of those affected), nausea, stomach pain, vomiting, and loss of appetite. These don’t show up after months-they hit fast. About two-thirds of people feel them within the first 30 days of starting the pill.
Here’s the thing: these symptoms aren’t a sign your body is rejecting the drug. They’re a reaction to how metformin works. It changes the way your gut bacteria behave and slows down sugar absorption in the intestines. That leads to gas, bloating, and loose stools. It’s not an allergy. It’s a side effect-and it usually fades.
Studies show that 85% of people who experience these issues see them disappear within 2 to 4 weeks. But waiting that long without relief can be miserable. So what can you do?
- Switch to extended-release (ER) metformin. It releases slowly, so less hits your gut at once. People who switch report up to 43% fewer stomach problems.
- Take it with food. Always. Even if you’re not hungry. A small snack with your pill makes a big difference.
- Start low, go slow. Instead of jumping to 1,000 mg a day, begin with 500 mg once daily. After a week, increase to 500 mg twice a day. Give your body time to adjust.
One Reddit user, who’s had type 1 diabetes since 2008, wrote: “I started with 500 mg ER at dinner. My diarrhea went from 4-5 times a day to just occasional cramping in 10 days.” That’s not magic. That’s smart dosing.
Lactic Acidosis: The Real Risk (And Why It’s Not What You Think)
Metformin carries a black box warning from the FDA-the strongest possible. It’s for lactic acidosis. That sounds terrifying. And it is. But here’s the truth: you’re far more likely to be struck by lightning than develop lactic acidosis from metformin.
The actual risk? Between 1 and 9 cases per 100,000 people each year. That’s rarer than being diagnosed with a rare form of cancer. And most of those cases happen in people who already have serious health problems.
Lactic acidosis isn’t caused by metformin alone. It’s caused by metformin + something else. Usually: kidney failure, liver disease, heart failure, severe infection, or heavy alcohol use. In fact, 93% of reported cases involve patients with at least one major risk factor.
What are the warning signs? If you feel extreme fatigue, rapid shallow breathing, muscle pain, or nausea that won’t go away-don’t wait. Go to the ER. These aren’t mild symptoms. They’re red flags. Laboratory tests will show: arterial pH below 7.35, lactate levels above 5 mmol/L, and an anion gap over 12.
And yes, the death rate for confirmed cases is high-30% to 50%. But here’s the critical point: almost all of those patients were critically ill in the hospital. They had sepsis, organ failure, or were in shock. Metformin didn’t kill them. Their underlying illness did. The drug just made it harder for their bodies to clear lactate.
Dr. Kenneth Cusi, a top endocrinologist, put it plainly: “The 50% mortality rate applies only to critically ill patients with multiple organ failures, not to stable outpatients on appropriate dosing.”
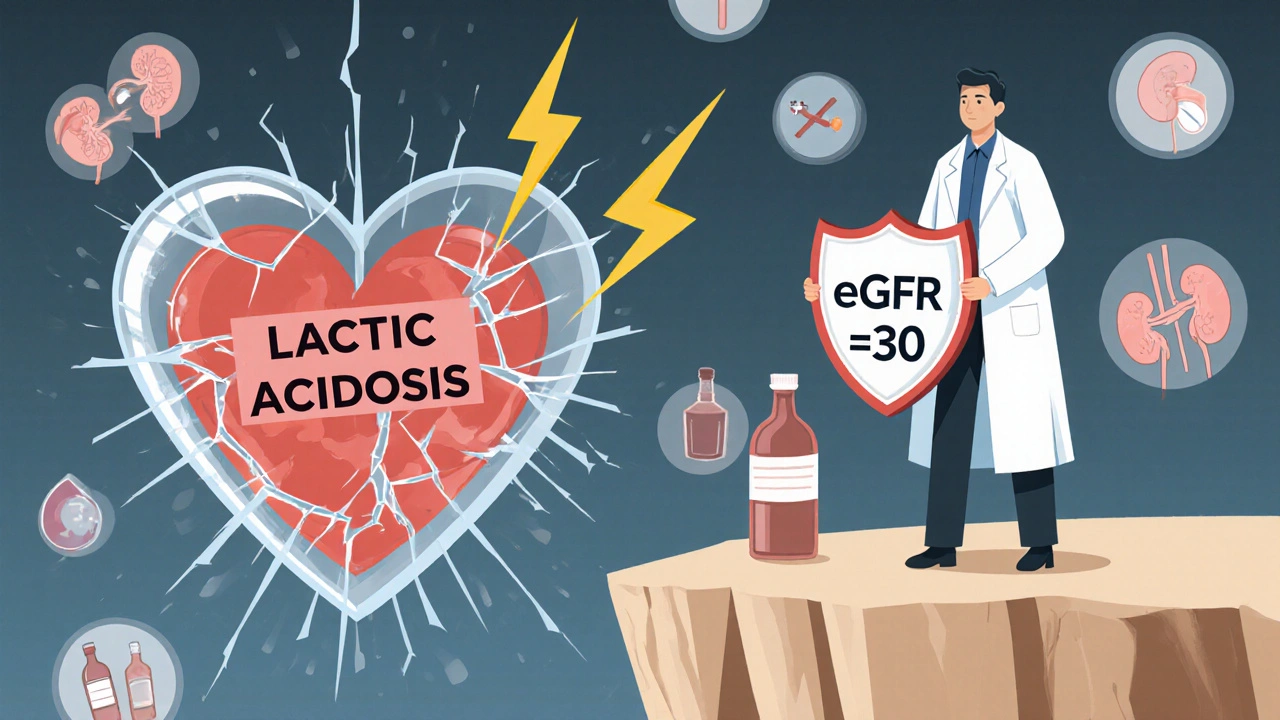
Who Should Not Take Metformin
Metformin isn’t for everyone. There are clear, non-negotiable rules.
- Don’t take it if your eGFR (kidney function) is below 30 mL/min/1.73m². At that point, your kidneys can’t clear the drug, and lactate builds up.
- Absolute no-go if your serum creatinine is above 1.4 mg/dL for men or 1.1 mg/dL for women. These are hard cutoffs set by the European Medicines Agency.
- Stop metformin 48 hours before any procedure involving contrast dye (like a CT scan). Restart only after your kidneys are confirmed to be working normally.
- If you’re over 80 and have other health issues, your doctor should be extra cautious.
- Don’t drink more than 3 alcoholic drinks a day. Alcohol and metformin together increase lactate production and reduce clearance.
Many people think metformin damages kidneys. It doesn’t. Studies show no increased risk of kidney decline over 10 years. Others worry it causes dementia or permanent vitamin B12 loss. It doesn’t cause dementia. And while it can lower B12 levels slightly in about 7% of long-term users, that’s easily fixed with annual blood tests and supplements.
What’s New in Metformin (2025 Update)
The FDA approved a new version of metformin in May 2023: Metformin-ER-XR. It’s designed to reduce stomach upset by 43% compared to older formulations. Early users report less bloating, fewer bathroom trips, and better tolerance overall.
Meanwhile, the TAME trial-funded by the NIH with $72 million-is still running. It’s testing whether metformin can delay aging-related diseases. But don’t rush to take it for longevity. The American Federation for Aging Research warns: “Current evidence does not support off-label use for longevity.” Stick to your prescribed use: managing type 2 diabetes.
How to Stay Safe on Metformin
Metformin is one of the safest drugs ever prescribed for diabetes. But safety depends on you and your doctor working together.
- Get your kidney function checked every 3 to 6 months if your eGFR is between 45 and 59. If it’s below 45, check monthly.
- Report any new muscle pain, unusual tiredness, or breathing changes immediately.
- Always tell every doctor you see that you’re on metformin-especially before surgery or imaging tests.
- Don’t skip your annual B12 check. If levels are low, take a supplement. No need to stop metformin.
- If GI symptoms persist beyond 4 weeks, talk to your doctor about switching to extended-release or trying a different medication.
Most people who start metformin never have serious problems. The GI side effects are annoying but temporary. The lactic acidosis risk is real-but only in people with multiple severe health issues. For the vast majority, metformin remains the best first choice for controlling blood sugar-and doing it without weight gain or hypoglycemia.
If you’re on metformin and feeling fine? Keep taking it. If you’re struggling with side effects? There are solutions. Talk to your doctor. Don’t quit on your own. And don’t let fear stop you from using a drug that’s helped over 150 million people live longer, healthier lives.


Matthew Stanford
Started metformin last month. Diarrhea was brutal for the first week. Switched to ER and took it with a peanut butter toast-game changer. No more panic attacks before leaving the house.
Still take it with food. Always. Even if I’m not hungry. Trust me, your gut will thank you.
Olivia Currie
OMG YES. I thought I was dying. Four times a day in the bathroom? I was crying in the stall at work. Then my endo said ‘try ER’ and I was like ‘is this real life?’-and it was. 10/10 recommend. My stomach finally stopped staging a rebellion.
Also, snacks. Always snacks. Even if it’s a single almond. It matters.
Curtis Ryan
metformin is the best thing ever for my sugar but my stomach was like ‘bro we out here’ for like 3 weeks. started at 500mg then went to 1000 after a week. now i feel like a normal human. no more bloating. no more panic. just chill.
also i take it with my coffee and a granola bar. works like magic. dont skip the food part. its not optional.
Rajiv Vyas
They say it’s safe. But why is it so cheap? Why is it pushed on everyone? Big Pharma doesn’t care about your gut-they care about your monthly refill. Lactic acidosis? Yeah, they downplay it. You think your kidneys are fine? Wait till you’re 70 and on 10 meds. Then you’ll see.
They don’t tell you about the B12 drop until you’re numb in your fingers. And then they hand you a $20 supplement. Classic.
farhiya jama
I just stopped it. Too much drama. My body was screaming. My doctor said ‘give it time’-but my time is valuable. I’m not a lab rat. I switched to GLP-1. Now I’m losing weight and not crying in the bathroom. Win-win.
Metformin is not for everyone. Stop gaslighting people who can’t tolerate it.
Astro Service
Why are we letting foreigners tell us how to take medicine? This drug was made in America. Why are we listening to some Indian doctor’s opinion? We don’t need your ‘eGFR’ nonsense. I’m healthy. I take it with my steak and beer. No problem.
Stop overcomplicating things. Just take the pill. America strong.
DENIS GOLD
Oh wow, a black box warning? And you’re telling me it’s safe? 😂
My cousin took metformin and now he’s on dialysis. Coincidence? I think not.
They don’t want you to know the truth. It’s all about the profit, baby.
Ifeoma Ezeokoli
I’ve been on this for 7 years. My stomach never bothered me. But I do take it with dinner, always. And I check my B12 yearly. Simple. No drama.
People panic over side effects like it’s a horror movie. It’s medicine. Not a curse. Chill. Your body adapts.
Also-yes, the ER version is better. I switched in 2021. Life changed.
And no, it didn’t kill my kidneys. My kidneys are fine. I’m 62. Still hiking.
Trust your doc. Not Reddit.
Daniel Rod
Just wanted to say-this post made me feel seen. 😊
I was terrified of metformin. Thought I was going to die from lactic acidosis. Then I read the stats. 1 in 100,000? That’s less than being hit by a vending machine falling off a truck.
And the GI stuff? Yeah, it sucks. But it’s like teething for adults. Painful. Temporary. And honestly? Worth it.
My HbA1c dropped from 8.2 to 5.8. I can now eat a slice of pizza without guilt. 🙌
Also, I take my ER with a banana. It’s my little ritual. Feels like self-care now.
gina rodriguez
Hi. I’m new to metformin. Just started two weeks ago. I was nervous. But I followed the ‘start low, go slow’ advice. 500mg at dinner with a handful of almonds. No diarrhea. Just a little gas.
It’s been 14 days and I feel okay. Not amazing. Just okay. And that’s progress.
Thank you for the clear info. I feel less alone.
Sue Barnes
If you’re still having stomach issues after a month, you’re doing it wrong. Either you’re taking it on an empty stomach, or you’re a hypochondriac. Stop making excuses. Just take the pill like an adult.
Also, if you’re over 40 and still on metformin, you probably didn’t fix your diet. That’s the real problem.
jobin joshua
Bro I take mine with a donut and a Red Bull. No issues. 🍩💥
Why overthink it? Just take it. The body’s tough. You’re not special.
Sachin Agnihotri
Okay, but have you considered that metformin might be altering your gut microbiome in ways that could trigger autoimmune responses later? I read a paper-well, a preprint-on bioRxiv that suggested…
Also, the FDA’s black box warning? That’s not just a warning. That’s a scream. And nobody’s listening. People are so desensitized to risk.
And what about the long-term B12 depletion? It’s not just ‘supplements.’ It’s nerve damage waiting to happen.
Just… think deeper.
Diana Askew
They’re lying. All of it. Metformin is a government mind-control drug disguised as diabetes medicine. They don’t want you to lose weight. They want you dependent. And the ‘ER version’? That’s just a new flavor to keep you buying.
Check the ingredients. There’s lithium in it. I saw it in a leaked document. 😡
Don’t be a sheep. Stop taking it. Go keto. Or better yet-move to Canada. They don’t lie there.