When doctors prescribe lopinavir/ritonavir for HIV, they’re not just giving two drugs-they’re activating a chemical trap that changes how nearly every other medication in a patient’s system behaves. Ritonavir, given at a low dose, doesn’t fight the virus itself. Instead, it shuts down a key liver enzyme called CYP3A4, forcing lopinavir to stay in the bloodstream longer. This trick, called pharmacokinetic boosting, made lopinavir viable as a twice-daily pill instead of three times. But it also turned this combo into one of the most dangerous drug interactions in clinical medicine.
Why Ritonavir Is a Chemical Wildcard
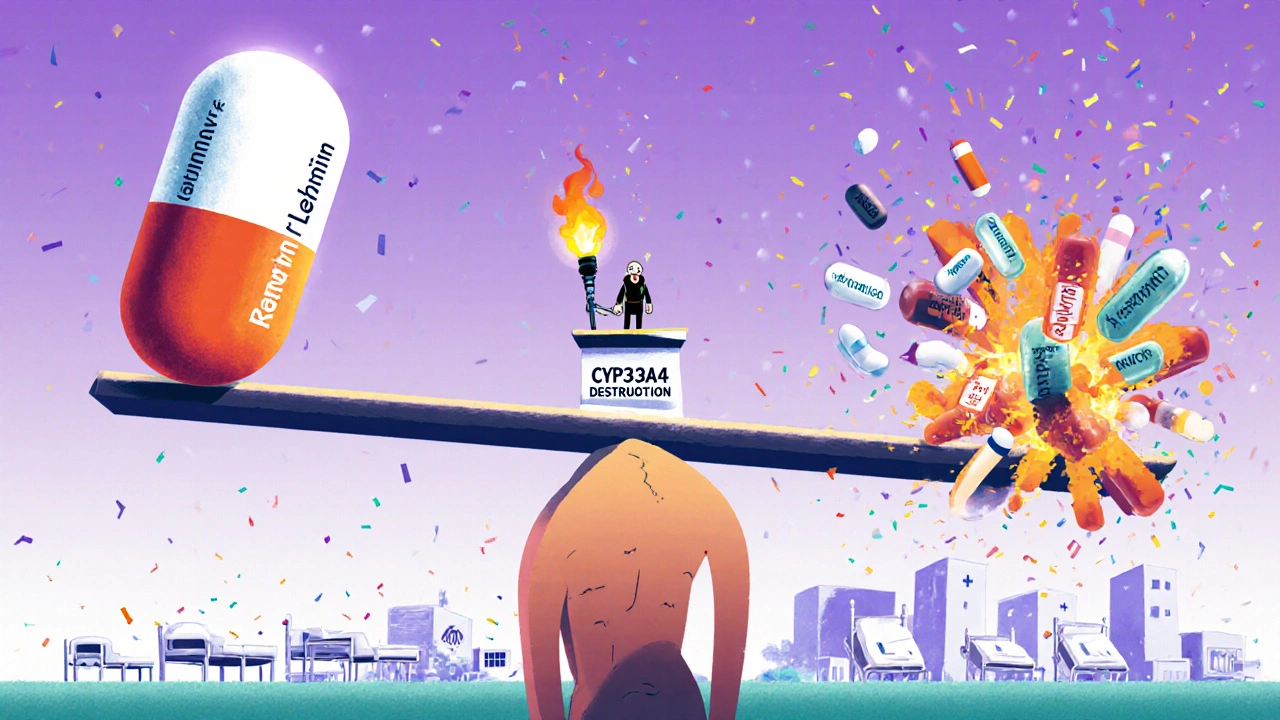
Ritonavir doesn’t just block CYP3A4-it breaks it. Unlike simple inhibitors that temporarily bind to the enzyme, ritonavir destroys it. It forms tight complexes with the enzyme’s heme group, damages the heme itself, and even sticks reactive pieces of itself to the enzyme’s protein structure. This isn’t a pause button. It’s a demolition job. And because CYP3A4 handles about half of all prescription drugs, this single action can send ripples through a patient’s entire medication list.
Without ritonavir, lopinavir clears from the body in under 7 hours. With it, that half-life stretches to over 12 hours. That’s the goal. But ritonavir doesn’t stop at CYP3A4. It also blocks CYP2D6, which metabolizes antidepressants, beta-blockers, and some pain meds. At the same time, it turns on CYP1A2, CYP2B6, CYP2C9, and CYP2C19-enzymes that break down warfarin, statins, and even birth control pills. This isn’t a simple boost. It’s a seesaw: one drug goes up, another crashes.
The Numbers That Scare Clinicians
The Liverpool HIV Interactions Database, updated in July 2023, lists 1,247 potential drug interactions with lopinavir/ritonavir. That’s more than any other antiretroviral combo. For comparison, darunavir/cobicistat has under 900. And it’s not just a theoretical risk.
- Midazolam, a sedative used in surgery, can reach 500% higher blood levels when taken with ritonavir. That’s not a side effect-it’s a near-certain overdose if doses aren’t cut by 60-80%.
- Fentanyl exposure increases 300%. Anesthesiologists now treat patients on ritonavir as high-risk surgical cases.
- Rivaroxaban, a blood thinner, is outright contraindicated. The risk of fatal bleeding is too high.
- Tacrolimus, used after organ transplants, requires a 75% dose reduction. One wrong calculation can lead to kidney failure or rejection.
- Warfarin’s effectiveness drops because ritonavir turns on CYP2C9. INR levels can swing wildly without warning.
A 2008 study showed that giving rifampicin (a TB drug) to someone on lopinavir/ritonavir slashed lopinavir levels by 76%. The result? A jump in liver toxicity from 11% to 33%. That’s not a rare side effect. That’s a predictable disaster.
What Happens When the Boost Fails
The biggest myth about ritonavir boosting is that it’s foolproof. It’s not. If a patient starts taking rifampicin, St. John’s wort, or even some seizure meds like carbamazepine, the enzyme induction can overpower the inhibition. Lopinavir levels crash. The virus rebounds. Resistance builds. And because lopinavir has a narrow therapeutic window, even a 20% drop can mean treatment failure.
Even the timing matters. Ritonavir’s half-life is only 3-5 hours, but its effect on CYP3A4 lasts days. That’s why the so-called “Paxlovid rebound” happens in COVID-19 patients. Nirmatrelvir (the active antiviral) clears faster than ritonavir. Once ritonavir’s effect fades, the body starts breaking down nirmatrelvir again-and the virus comes back. The same logic applies to lopinavir. If a patient misses a dose or starts a new drug that induces CYP3A4, the boost collapses.
Who Still Gets It-and Why
In the U.S., lopinavir/ritonavir is rarely used anymore. Since 2015, guidelines have pushed doctors toward integrase inhibitors like dolutegravir. They’re simpler, safer, and have fewer interactions. Only 5% of new HIV prescriptions in the U.S. now use lopinavir/ritonavir.
But in low- and middle-income countries, it’s still common. Why? Cost. In PEPFAR programs, a year’s supply costs $68 per person. Dolutegravir? $287. That’s a 76% difference. For countries treating millions, price wins over safety. UNAIDS estimates that in 2022, lopinavir/ritonavir was still used in 28% of first-line HIV regimens in these regions.
It’s also still used in kids. Some pediatric formulations aren’t available for newer drugs. And in cases of multi-drug resistance, it’s one of the few options left.
The Hidden Risk: Hormonal Birth Control
One of the most overlooked dangers is contraception. Ritonavir induces CYP3A4 and CYP2C19-enzymes that break down estrogen and progestin. Studies show hormonal birth control becomes less than 50% effective in patients taking lopinavir/ritonavir. Many women don’t know this. Clinicians sometimes forget to ask.
The result? Unplanned pregnancies. In 2021, a case report from South Africa described a woman on lopinavir/ritonavir who became pregnant despite using the pill. She was told the pill was fine. It wasn’t. Backup methods aren’t optional-they’re mandatory.
How to Avoid a Dangerous Interaction
If someone is starting lopinavir/ritonavir, here’s what must happen:
- Run a full medication review. Include over-the-counter drugs, supplements, and herbal products. St. John’s wort? Stop it. Rifampin? Avoid it.
- Check the Liverpool HIV Interactions Database. It’s free, updated monthly, and used by over 2.8 million clinicians annually.
- For drugs with known interactions, adjust doses before starting. Don’t wait for symptoms.
- For anticoagulants, statins, or immunosuppressants, monitor levels closely. INR, drug concentrations, kidney function-all need tracking.
- Warn patients: if they’re prescribed anything new-even an antibiotic or painkiller-tell their HIV doctor first.
There’s no shortcut. This isn’t like checking for aspirin and warfarin. This is a minefield. One missed interaction can kill.

The Future: Is There Still a Place for Ritonavir Boosting?
Yes-but only in specific cases. The real future of ritonavir isn’t in HIV. It’s in Paxlovid. The same boosting mechanism that made lopinavir work is now used to keep nirmatrelvir alive long enough to fight SARS-CoV-2. But even there, problems remain. Rebound cases, drug interactions, and variable metabolism mean it’s far from perfect.
Researchers are now studying CYP3A5 gene variants. Some people naturally produce more of this enzyme. Preliminary data shows they clear lopinavir 28% faster, meaning standard doses may not work for them. Personalized dosing based on genetics could be the next step-but it’s not here yet.
For now, lopinavir/ritonavir survives not because it’s the best, but because it’s cheap, available, and, when managed correctly, effective. But it demands respect. Every dose carries a hidden risk. Every patient needs a full interaction audit. And every prescriber must treat this combo like a live wire-handle with care, or someone gets hurt.
When to Avoid It Altogether
There are clear red flags. Don’t use lopinavir/ritonavir if the patient is taking:
- Alfuzosin (for enlarged prostate) - risk of severe low blood pressure
- Ergot derivatives (for migraines) - risk of limb ischemia
- Midazolam or triazolam (sedatives) - risk of respiratory arrest
- Rivaroxaban or apixaban - risk of major bleeding
- Voriconazole - unpredictable levels, risk of liver damage
- St. John’s wort or rifampin - treatment failure
These aren’t "use with caution" warnings. These are absolute contraindications. The FDA and EMA both list them as black box dangers.
Can lopinavir/ritonavir be used with statins?
Yes-but only certain ones. Rosuvastatin and pravastatin are safer because they aren’t primarily metabolized by CYP3A4. Atorvastatin and simvastatin are dangerous. Simvastatin can cause life-threatening muscle damage when boosted by ritonavir. If a statin is needed, switch to rosuvastatin or pravastatin and start at the lowest dose. Monitor for muscle pain and CK levels.
Why is ritonavir still used if it has so many interactions?
Because it works-and it’s cheap. In places where newer drugs cost $200-$300 per year, lopinavir/ritonavir costs under $70. For millions of people in low-income countries, that’s the difference between treatment and no treatment. It’s not ideal, but it’s life-saving. The trade-off is rigorous monitoring and strict avoidance of dangerous drug combinations.
Is there a safer alternative to ritonavir boosting?
Yes-cobicistat. It’s a pure CYP3A4 inhibitor with no induction effects. It doesn’t affect CYP2C9 or CYP1A2 like ritonavir does. Drugs like darunavir/cobicistat have far fewer interactions (around 890 vs 1,247) and are now the standard in the U.S. and Europe. But cobicistat is more expensive and not always available in resource-limited settings.
Can you take lopinavir/ritonavir with birth control?
Not safely. Hormonal birth control pills, patches, or rings become less than half as effective. The only safe options are non-hormonal methods: copper IUD, condoms, or sterilization. If someone is on lopinavir/ritonavir and wants to prevent pregnancy, they must use backup contraception-no exceptions.
What should I do if I’m on lopinavir/ritonavir and get prescribed a new drug?
Stop. Don’t take it. Call your HIV provider or pharmacist immediately. Even common drugs like antibiotics (e.g., clarithromycin), antifungals (e.g., fluconazole), or pain relievers (e.g., tramadol) can interact. Use the Liverpool HIV Interactions Database or ask for a formal drug interaction check. Never assume a new prescription is safe just because it’s not an HIV drug.
Final Thought: It’s Not the Drug-It’s the System
Lopinavir/ritonavir isn’t evil. It’s a tool. A powerful, blunt, dangerous tool. It saved lives when better options didn’t exist. It still does-in places where cost matters more than convenience. But it demands more than a prescription. It demands vigilance. It demands time. It demands that every doctor, pharmacist, and patient understand: one wrong pill can undo everything.


Esperanza Decor
This post is one of the most terrifyingly clear breakdowns of drug interactions I’ve ever read. I work in pharmacy and even I didn’t realize how deep the enzyme destruction goes with ritonavir. It’s not just inhibition-it’s molecular sabotage. The fact that it breaks CYP3A4 permanently until new enzymes are made changes how we think about dosing timelines. No wonder patients on this combo have such unpredictable reactions to antibiotics or even OTC pain meds.
Deepa Lakshminarasimhan
They’re hiding something. Why is this still used in poor countries? Why not just give them the real drugs? I’ve heard the cost argument, but what if the real reason is they don’t want people living too long? Look at how many deaths are just buried under "unexplained liver failure." This isn’t medicine-it’s a population control experiment dressed up as charity.
Erica Cruz
Wow. Someone actually wrote a 2000-word essay on ritonavir? Congrats, you just turned a pharmacokinetic footnote into a Netflix documentary. This isn’t groundbreaking-it’s textbook. If you’re prescribing this combo in 2024 without checking the Liverpool database, you shouldn’t be licensed. The fact that this even needs explaining is a tragedy of medical education.
Johnson Abraham
lol so ritonavir is like a drug bully? shuts down all the other meds? guess that’s why my cousin’s liver went nuts after he took it with his statin. dumbass doc didn’t even ask what else he was on. also why does everyone spell it "ritonavir" like it’s a spell from harry potter? its just a pill.
Shante Ajadeen
Thank you for writing this. I’m a nurse in a rural clinic and we still use this combo because it’s all we can afford. I’ve seen the confusion in patients’ eyes when we tell them they can’t take their anxiety med or birth control. This post helps me explain it better. I’m printing it out for our team.
dace yates
Does anyone know if the CYP3A5 genetic variants affect ritonavir boosting the same way they affect tacrolimus? I’ve read a few papers suggesting CYP3A5 expressors clear lopinavir faster, but I haven’t seen data on whether higher doses actually improve outcomes in those patients. Anyone have a link?
Danae Miley
The Liverpool database is not "free" in any meaningful sense-it’s a curated tool maintained by academic institutions with grants, and its data is proprietary in structure. Calling it "free" misrepresents the infrastructure behind it. Also, the claim that 2.8 million clinicians use it annually is unverified. Cite your source, or don’t make inflated claims. Precision matters in clinical communication.
Charles Lewis
It’s important to contextualize the continued use of lopinavir/ritonavir not merely as a cost-driven compromise but as a reflection of systemic inequities in global health infrastructure. In regions where supply chains are unreliable, where cold storage is inconsistent, and where digital prescribing tools are absent, the stability, shelf life, and oral bioavailability of this combination become critical advantages. The moral imperative isn’t to replace it with more expensive alternatives-it’s to build systems that make those alternatives accessible. Until then, dismissing this regimen as outdated ignores the lived reality of millions who depend on it.
Renee Ruth
Someone’s gonna die because of this. Mark my words. It’s not a matter of if-it’s when. I’ve seen it before. A patient on this combo takes a simple antibiotic for a sinus infection, goes into liver failure, and the family sues the clinic. The doctor says, "I didn’t know." But you should’ve known. This isn’t a rare case. It’s a waiting disaster. Why isn’t this on every EHR alert system? Why aren’t pharmacists required to flag it like they do with warfarin?
Samantha Wade
This is exactly why we need mandatory pharmacogenomic screening before initiating any boosted protease inhibitor regimen. The fact that we’re still prescribing this without checking CYP3A5 status in 2024 is unacceptable. We have the tools. We have the data. What we lack is the political will to implement them equitably. Let’s not romanticize cost-saving as "life-saving" when it’s really just triage dressed in humanitarian language.
Elizabeth Buján
it’s wild how one molecule can hold so much power. it’s not just chemistry-it’s a story of who gets to live, who gets to be safe, and who gets left with the old, dangerous tools because the world decided their life was cheaper. i’m not a doctor but i’ve seen people choose between medicine and food. this isn’t a clinical footnote. it’s a mirror.
Andrew Forthmuller
just one thing: if you’re on this combo, don’t take turmeric supplements. they mess with cyp3a4 too. i learned the hard way.
vanessa k
thank you for writing this. i’m a woman on lopinavir/ritonavir and no one ever told me my birth control wouldn’t work. i got pregnant. it was terrifying. i almost didn’t tell anyone because i felt stupid. but you’re right-it’s not my fault. it’s the system. please, if you’re reading this and you’re on this med: use a copper iud. don’t trust the pill. don’t trust the patch. just do it.