When a critical medication expires, it’s not just a paperwork issue-it’s a patient safety crisis. Imagine a ventilator-dependent patient in the ICU whose fentanyl infusion runs out. The vial is labeled expired: December 1, 2025. The pharmacy has no more in stock. The next dose is due in 45 minutes. What do you do?
This isn’t hypothetical. In Australian and U.S. hospitals alike, expired critical medications trigger real-time emergencies. Unlike routine prescriptions, drugs like neuromuscular blockers, vasopressors, sedatives, and anticonvulsants can’t be delayed. A missed dose can mean organ failure, seizures, or death. The key isn’t panic-it’s a clear, pre-planned system to swap out expired drugs safely and quickly.
Not All Expired Medications Are the Same
Some expired meds are low-risk. A bottle of expired ibuprofen? Probably still safe, just less potent. But when you’re dealing with critical medications, potency, stability, and pharmacokinetics matter. These are drugs where even small changes in dose or chemistry can have life-or-death consequences.
Examples include:
- Neuromuscular blockers (cisatracurium, rocuronium)
- Vasopressors (norepinephrine, epinephrine)
- Sedatives (midazolam, propofol)
- Antidotes (flumazenil, naloxone)
- Antibiotics for sepsis (vancomycin, piperacillin-tazobactam)
These aren’t just any drugs. They’re the backbone of ICU care. In fact, studies show ICU patients receive an average of 12-18 different medications per day. When one expires, the ripple effect can destabilize an entire treatment plan.
The Three-Tier Replacement System
Leading hospitals use a tiered approach-first-line, second-line, third-line-to replace expired drugs. This isn’t guesswork. It’s based on clinical evidence, pharmacology, and years of ICU experience.
For example, if cisatracurium (a neuromuscular blocker) expires:
- First-line: Rocuronium - same onset, similar duration, widely studied in ICU
- Second-line: Vecuronium - longer duration, less predictable in renal failure
- Third-line: Atracurium - metabolized differently, risk of histamine release
Why this order? Rocuronium has been tested in over 15,000 ICU patients. Its safety profile is predictable. Vecuronium is effective but slower to reverse. Atracurium? It can cause low blood pressure and itching-risky in unstable patients.
This system isn’t optional. The American Society of Health-System Pharmacists (ASHP) says every hospital with an ICU must have a written, approved list of therapeutic alternatives for critical drugs. And it’s not just for shortages. It applies to expiration, recalls, supply chain failures-any reason the drug becomes unavailable.
Who Decides? Pharmacists Are the Linchpin
Doctors don’t pick replacements on the fly. Nurses don’t guess. It’s the pharmacist-specifically, the critical care pharmacist-who leads the decision.
They run a 4-step check:
- Validate the expiration: Is it truly expired? Was it stored correctly? Some meds last longer if refrigerated.
- Check inventory: Do we have any left? Is it usable? Sometimes a vial is expired but still within stability limits.
- Match to patient: Is the patient on renal dialysis? Liver disease? Allergies? A drug safe for one person might kill another.
- Choose the tier: Select the best alternative from the approved list, then adjust the dose.
Studies show hospitals with dedicated critical care pharmacists reduce medication errors by 41% and cut ICU stays by 2.3 days on average. One hospital in Melbourne cut its medication-related readmissions by 27% after hiring two full-time pharmacists for its ICU.
But here’s the problem: only 42% of community hospitals have a pharmacist on-site 24/7. In rural clinics or smaller facilities, nurses and doctors are left to make these calls alone. That’s when mistakes happen.
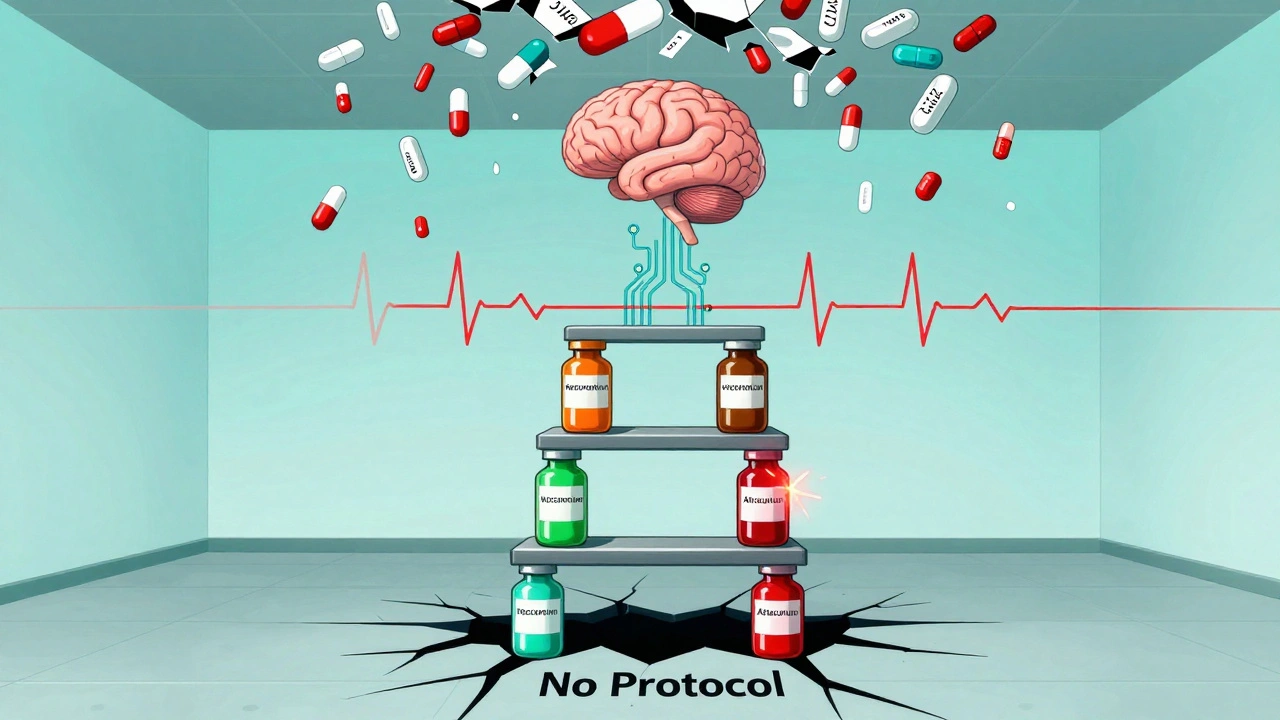
What Happens When There’s No Plan?
In 2024, a survey of 1,200 U.S. hospitals found that 53% had no written protocol for expired critical medications. Some used “first come, first served.” Others flipped a coin. One hospital even used a lottery system during a multi-drug shortage.
Results? Patients got the wrong dose. Sedatives were swapped for ones that didn’t match their pain level. Vasopressors were replaced with less potent versions-leading to prolonged low blood pressure and kidney damage.
One case from a regional hospital in Queensland: a patient on expired norepinephrine was switched to phenylephrine without dose adjustment. His blood pressure spiked to 210/110. He suffered a stroke. The hospital paid $2.1 million in settlement.
These aren’t rare. The Joint Commission found medication errors linked to expired or unavailable drugs were cited in 68% of serious safety events in 2024. That’s up from 59% in 2022.
How to Build a Replacement Protocol
If you’re in a hospital, clinic, or pharmacy, here’s how to create a system that works:
- Identify your critical drugs. List every medication that could cause harm if delayed. Include doses, routes, and typical patient populations.
- Assign tiers. For each drug, list 1st, 2nd, and 3rd alternatives. Use ASHP guidelines and peer-reviewed studies. Don’t guess.
- Build order sets. Create pre-written electronic orders for each alternative. One click, no typing errors.
- Train your team. Run monthly drills. Simulate an expiration event. Time how long it takes to switch.
- Automate alerts. Use pharmacy software that flags drugs expiring in 30 days. Some systems even auto-suggest replacements.
High-performing hospitals also have a daily medication review team: pharmacist, nurse, doctor, and clinical pharmacist. They meet for 15 minutes every morning to check for expirations, shortages, or high-risk switches.

Technology Is Changing the Game
AI tools are now being tested to recommend replacements. One system at the University of Colorado analyzed 147 patient variables-age, weight, kidney function, liver enzymes, current meds, allergies-and matched expired drugs with the safest alternative 95% of the time. It matched expert pharmacists’ choices nearly perfectly.
Meanwhile, inventory systems now track expiration dates in real time. Some can even auto-order replacements when stock hits 10%. In Sydney, one hospital reduced expired meds by 76% in 18 months using this system.
The FDA is also looking at extending expiration dates for certain drugs based on stability testing. If approved, this could cut waste by 20%. But until then, your protocol must assume expiration = unusable.
What You Can Do Today
If you’re a clinician, pharmacist, or hospital administrator, here’s what to do right now:
- Find your top 5 critical medications. Write down their alternatives.
- Ask your pharmacy: Do we have a written replacement protocol? If not, start one.
- Check your inventory: Are any critical drugs expiring in the next 30 days?
- Train your team. Even a 20-minute huddle can prevent a disaster.
Don’t wait for someone else to fix it. The system is broken in too many places. But it’s fixable-with a plan, a pharmacist, and a little preparation.
Expired meds aren’t just a logistics problem. They’re a test of your team’s readiness. The difference between a smooth switch and a patient crisis? A checklist. A protocol. A person who knows what to do before the clock runs out.
What should I do if a critical medication expires and I don’t have a replacement on hand?
Don’t delay. Immediately contact your pharmacy or clinical pharmacist. Use your hospital’s approved therapeutic alternatives list. If none are available, escalate to the on-call critical care team. Never use an unapproved substitute. If you’re in a rural or under-resourced setting, contact your regional health network-they may have emergency stock or transfer protocols. Time matters, but safety matters more.
Can I still use an expired medication if it looks fine?
No. Even if the liquid looks clear or the tablet isn’t discolored, potency and chemical stability can’t be guaranteed after the expiration date. For critical medications like vasopressors or sedatives, even a 10% drop in potency can lead to under-treatment. In septic shock, that could mean the difference between life and death. Never use expired critical drugs-regardless of appearance.
Why can’t I just use a similar drug I’ve used before?
Drugs that seem similar aren’t interchangeable. For example, switching from fentanyl to morphine in an ICU patient requires a 3:1 dose conversion-but even that isn’t exact. Morphine has active metabolites that build up in kidney failure. Fentanyl doesn’t. One patient might tolerate the switch. Another could stop breathing. Only a pharmacist, using patient-specific data and approved guidelines, can safely determine if a substitution works.
How do I know which alternative is best for a patient with kidney disease?
For patients with kidney failure, avoid drugs cleared by the kidneys. For example, vecuronium and morphine can accumulate. Cisatracurium and fentanyl are safer because they break down by other pathways. Always check the pharmacokinetics of the alternative. Your hospital’s replacement protocol should include special notes for renal, hepatic, or geriatric patients. If it doesn’t, ask your pharmacy to add them.
Are there any free resources to help build a replacement protocol?
Yes. The American Society of Health-System Pharmacists (ASHP) offers free guidelines on drug shortage management, which apply directly to expired medications. The FDA also maintains a Drug Shortages database. Many hospitals share their protocols through professional networks. Start with ASHP’s 2023 Guidelines and adapt them to your facility’s needs. You don’t need to build from scratch-just customize what already works.
What’s Next? The Future of Medication Safety
By 2027, 76% of healthcare systems plan to have unified, AI-assisted replacement protocols. That means real-time alerts, automated substitutions, and instant access to expert guidance-all built into the electronic health record.
But technology won’t replace judgment. It will support it. The best systems still rely on pharmacists who understand not just the drugs, but the patient. The person behind the chart. The family waiting outside. The nurse who noticed the patient’s breathing changed after the switch.
Expire dates don’t lie. But our systems do-if we let them. The solution isn’t more drugs. It’s better processes. Clear roles. Trained teams. And a culture that treats medication safety like a life-or-death emergency-because it always is.


Ruth Witte
This is literally life or death stuff 😭 I can't believe some hospitals are still flying blind. Someone's kid could die because no one had a damn protocol. 🚨
Noah Raines
Been there. Saw a nurse swap fentanyl for morphine without adjusting the dose. Patient coded. Took 17 minutes to get the right med. We got lucky. Don't be that guy.
Delaine Kiara
Oh please. You think this is new? I worked in a rural ER in 2018 where they used expired epinephrine because the pharmacy was closed. The patient lived. So chill. Not everything is a crisis. 🙄
Lauren Dare
Let me guess - the 'critical care pharmacist' is the same person who also handles the vending machine inventory and answers the phone at 3am. 😒 The system is designed to fail. We're outsourcing life-or-death decisions to overworked, underpaid clerks with a PharmD on their wall.
Andrea Petrov
You know who really controls the drug supply? Big Pharma. They let meds expire on purpose so they can jack up prices. The FDA? They're in the pocket. That's why they're 'considering' extending expiration dates - it's a PR stunt. Real safety? Never coming. They want you dependent on their overpriced, short-supply nonsense.
Graham Abbas
There's something profoundly human here, isn't there? We've built these towering cathedrals of medicine - algorithms, protocols, AI, tiered alternatives - yet the moment the vial expires, it all collapses back to a single person, in a dim room, holding a syringe, wondering if they're about to kill someone. The real technology isn't the software. It's the courage of the pharmacist who says, 'I'll take responsibility.'
Angela R. Cartes
Wow. So much text. Can we just say 'use the ASHP guidelines' and call it a day? I'm tired. 🥱
Andrea Beilstein
I think the real issue is we treat meds like they're batteries with expiration dates when they're more like relationships - they need context to matter. A drug isn't dangerous because it's expired. It's dangerous because we stopped seeing the person behind the chart. The vial doesn't care about your protocol. The patient does
iswarya bala
this is so important!! i work in a small clinic in india and we have no pharmacist on site. we rely on drs and nurses to make calls. thank you for sharing this. i will start making a list right now 💪
Tim Tinh
Man I just read this after my shift. We had a propofol shortage last week. We used midazolam instead. Didn't have the full protocol ready. We got lucky. But I'm printing this out. Gonna put it on the fridge. My team needs to see this. Thanks for writing this.
Philippa Barraclough
I'm curious - how many of these tiered replacement protocols have been validated in prospective, randomized trials? Or are they largely based on expert opinion and institutional inertia? Because while the intent is noble, I worry that in the absence of robust evidence, we're creating a false sense of security. For instance, switching from cisatracurium to rocuronium may seem straightforward, but the pharmacokinetic differences in septic patients with capillary leak syndrome are non-trivial. Are we really accounting for that in every hospital's protocol? Or are we just copying what the big academic centers do and assuming it's universally applicable? The risk of therapeutic substitution isn't just about potency - it's about hidden, context-dependent variables that no checklist can fully capture.