Every month, pharmacists face the same challenge: patients showing up for a refill before they should. Some claim their insurance allows it. Others say their doctor wrote it. A few even offer to pay cash, thinking that clears the way. But behind these requests often lie hidden dangers - early refills that lead to overdose, duplicate prescriptions that cause toxic interactions, and broken systems that let mistakes slip through. These aren’t just inconveniences. They’re medication safety failures that can land people in the ER - or worse.
The truth is, early refills and duplicate therapy aren’t random. They’re predictable patterns. And when pharmacies treat them as surprises instead of system failures, patients pay the price. The good news? You can stop these mistakes before they start. It doesn’t require fancy tech or huge budgets. It takes clear protocols, trained staff, and a mindset shift: refills aren’t emergencies - they’re scheduled events.
Understand Why Early Refills Happen
Most patients don’t try to game the system. They’re confused. Insurance plans often say you can get a 30-day supply "5 days early." Many patients hear that as "I can use up my meds 5 days early, then refill." That’s not how it works. The 5-day window is meant for travel or emergencies - not to stretch out your supply. But without clear communication, patients assume they’re entitled to refill early every time.
Then there’s the real problem: patients using multiple pharmacies. A person on pain meds might get one script from their primary care doctor, another from a specialist, and a third from a pharmacy across town. If those pharmacies don’t talk to each other, duplicate therapy slips through. One pharmacist sees a prescription for oxycodone. Another sees a separate one for hydrocodone. Neither knows the patient is doubling up. The result? Respiratory depression. Hospitalization. Death.
Controlled substances make this worse. DEA rules say Schedule II drugs - like oxycodone, fentanyl, or Adderall - can’t be refilled at all. But some patients still try. They’ll call multiple prescribers. They’ll claim their prescription was lost. They’ll say they "ran out early" because of work stress. Without a system to catch these patterns, you’re not just filling a prescription - you’re enabling misuse.
Build a Risk-Based Refill Protocol
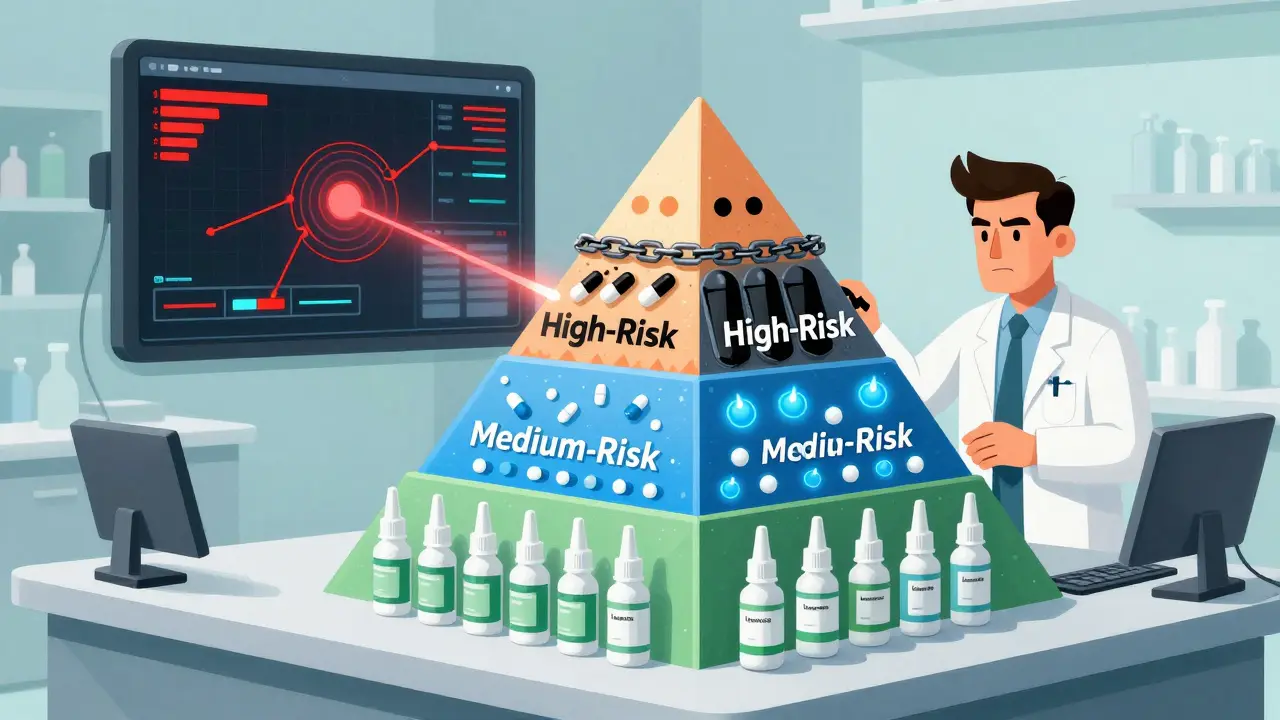
Not all medications are equal. A nasal spray for allergies? Low risk. A blood thinner? High risk. A controlled painkiller? Highest risk. Your refill protocol should reflect that.
Start by grouping medications into three tiers:
- Low-risk: Things like nasal steroids, thyroid meds, or antihistamines. These can be auto-approved if the patient has been seen in the last 6 months.
- Medium-risk: Blood pressure pills, diabetes meds, or birth control. These can be refilled for up to 90 days if the patient has had labs or a visit in the last 90 days. Let nurses or medical assistants handle these approvals.
- High-risk: Opioids, benzodiazepines, stimulants. These require direct provider approval every time. No exceptions.
One health system saw a 78% drop in provider workload after implementing this system. Nurses approved 64% of refill requests automatically. Only 18% needed a doctor’s sign-off. That’s not just efficient - it’s safer.
Use Your EHR Like a Safety Net
Your Electronic Health Record (EHR) isn’t just for charting. It’s your frontline defense against duplicate therapy and early refills.
Set up automated alerts. If a patient requests a refill 7 days before their last one was filled, the system should flag it. If they’ve had two opioid prescriptions from different doctors in the last 30 days, it should stop the refill and notify the prescriber.
Also, use EHR notes to track refill history. When a patient gets a refill early, add a note: "Refilled 3 days early on 2/12/2026 - patient reported lost bottle." That way, next time, the pharmacist sees the pattern. Don’t rely on memory. Rely on data.
And don’t forget the clinical viewer. In Australia, systems like My Health Record and state-based prescription monitoring tools let pharmacists see what’s been dispensed elsewhere. If a patient fills a script at a pharmacy in Melbourne and another in Sydney, you’ll know. That’s how you catch duplicate therapy.
Train Your Team to Ask the Right Questions
Pharmacists aren’t cops. But you are the last line of defense. And that means asking questions - not just scanning barcodes.
When someone asks for an early refill, don’t say "No." Say: "Can you tell me what happened?"
Maybe they lost the bottle. Maybe they ran out because they forgot to take it. Maybe they’re using it for anxiety and their doctor didn’t realize. The answer changes your response.
Train your staff to look for red flags:
- Asking for cash only
- Claiming the prescription was "written by a different doctor"
- Coming in right after a weekend or holiday
- Refusing to let you call the prescriber
Also, check for gaps. If a patient hasn’t picked up a refill in 4 months and suddenly shows up for 3 bottles - that’s not compliance. That’s stockpiling. Talk to them. Call the prescriber. Don’t assume.
Set Clear Policies - and Stick to Them
One pharmacy in Sydney stopped early refills for controlled substances cold. No exceptions. Not even for "emergencies." The rule? Two days early, max. And even then, only if the prescriber confirms.
It sounds strict. But here’s what happened: early refill requests dropped 82%. Patient complaints? Fewer than before. Why? Because patients learned: this pharmacy doesn’t play games.
Write your policy. Post it. Train every staff member on it. Include:
- Maximum early refill window (e.g., 2 days for controlled substances, 5 days for others)
- When provider approval is required
- How to handle patients who insist on cash
- How to check for duplicate therapy using monitoring tools
And make sure everyone knows: if a patient threatens to go elsewhere, you don’t bend. You say: "I want you to be safe. Let me help you talk to your doctor."

Make Refills Predictable - Not Reactive
The biggest mistake? Waiting for patients to call.
Think of refills like a train schedule. If you know someone needs a refill every 30 days, don’t wait for them to ask. Proactively prepare it.
Doctors can sign prescriptions in advance. If they’re going on vacation, they can authorize a refill for their patients. Nurses can send reminders: "Your next refill is due on March 10. Would you like us to prepare it?"
One practice in Perth cut refill-related ER visits by 40% just by sending automated text reminders. Patients didn’t run out. They didn’t panic. They didn’t seek early refills.
Technology Is Your Ally - Not Your Replacement
Yes, CDS tools help. Yes, prescription monitoring programs catch patterns. But tech alone won’t stop a patient who says, "I just need one more pill - I’m in pain."
What works? A system where:
- Technology flags risks
- Staff are trained to respond
- Policies are clear and enforced
- Prescribers and pharmacists talk
That’s how you stop early refills. That’s how you stop duplicate therapy. That’s how you save lives.
Can I refill a Schedule II controlled substance early?
No. Under DEA regulations, Schedule II drugs - such as oxycodone, fentanyl, and Adderall - cannot be refilled under any circumstances. Even if the patient claims they lost the prescription, ran out early, or need it for an emergency, a new prescription must be written. Pharmacies that refill these drugs without a new script risk legal penalties and endanger patient safety.
How do I know if a patient is getting duplicate therapy?
Use your pharmacy’s clinical viewer or state prescription monitoring program. These tools show prescriptions filled at other pharmacies. Look for overlapping drugs with similar effects - like two different opioids, or two benzodiazepines. Also check for timing: if a patient fills a script for gabapentin on Monday and another for pregabalin on Wednesday, they’re likely doubling up. Always verify with the prescriber before dispensing.
What should I do if a patient insists on an early refill and offers to pay cash?
Don’t accept cash as a reason to override policy. Politely explain that your pharmacy follows safety protocols to protect patients - not just insurance rules. Say: "I can’t fill this early, even if you pay cash, because it could be dangerous." Then offer to contact the prescriber with them. Most patients will accept that. If they refuse, document the interaction and report the behavior to your state’s prescription monitoring program.
How can I reduce the number of refill calls from patients?
Set up automated refill reminders via text or email. Let patients know their refill is ready 3-5 days before it’s due. For chronic meds, offer 90-day supplies with prior authorization. Train staff to ask: "Would you like us to prepare your next refill now?" This turns reactive calls into proactive service. One pharmacy reduced refill calls by 60% using this approach.
Is it okay to refill a medication if the patient says their doctor told them they could?
No. Always verify. Patients sometimes misunderstand what their doctor said. Or they confuse one prescriber with another. Or they’re repeating misinformation. Your responsibility is to check the prescription against your records and, if needed, call the prescriber directly. Never assume. Always confirm. It’s not about distrust - it’s about safety.


Write a comment