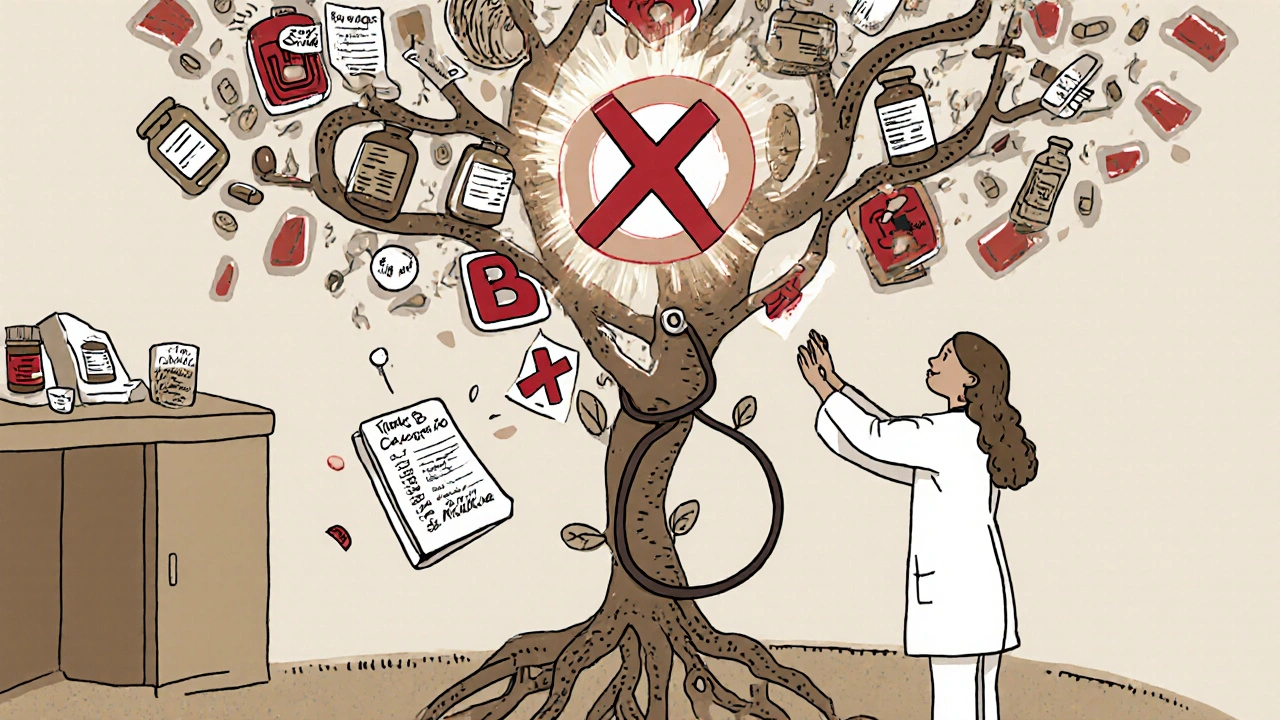
Why Talking About Medications with Your OB/GYN Isn’t Optional
Most women assume their OB/GYN already knows what they’re taking - but that’s a dangerous assumption. You might think your daily vitamin, herbal tea, or over-the-counter painkiller is harmless. But during pregnancy or breastfeeding, even something as simple as ibuprofen or St. John’s Wort can have real consequences. The truth is, your OB/GYN needs to know everything - not just prescriptions, but supplements, cannabis, alcohol, and even the herbal remedies your grandmother swore by.
According to the CDC, about 90% of pregnant women take at least one medication during pregnancy. And nearly 70% continue taking drugs they were on before getting pregnant - things like thyroid meds, antidepressants, or blood pressure pills. But here’s the catch: many of these drugs weren’t tested on pregnant women. That means your provider has to make smart, informed calls based on the best available evidence. And they can’t do that unless you give them the full picture.
What You Need to Bring to Your Appointment
Don’t rely on memory. Don’t guess dosages. Don’t say “I think it was 200 mg.” Write it down. Here’s exactly what to include in your list:
- Prescription drugs: Name, dose, frequency, and purpose. Example: Levothyroxine 75 mcg, one pill daily, for hypothyroidism.
- Over-the-counter meds: Ibuprofen, acetaminophen, cold pills, antacids - even if you only take them once a month.
- Supplements: Prenatal vitamins, iron, omega-3s, magnesium, vitamin D. Include brand names if possible.
- Herbal products: Evening primrose oil, ginger capsules, red raspberry leaf tea. Yes, even those.
- Recreational substances: Alcohol, nicotine, cannabis. This isn’t judgment - it’s safety. If you’re using medical marijuana, tell them. It affects fetal development and breastfeeding.
Pro tip: Take photos of your medicine bottles with your phone. That way, if you forget a name or dose, you’ve got a visual backup. Many OB/GYN clinics now ask patients to upload this info before the appointment - some even have apps like Babyscripts that let you log meds in real time.
What Your OB/GYN Will Ask (And Why)
Your OB/GYN isn’t just checking boxes. They’re looking for risks. Here’s what they’re really trying to find out:
- Are you taking anything that could harm a developing baby? Some drugs are known teratogens - meaning they can cause birth defects. Accutane (isotretinoin) is a classic example. But others, like certain antidepressants or seizure meds, carry smaller but still real risks. Your provider will weigh those against the danger of stopping the drug.
- Are you on a medication that needs a dose change? Pregnancy changes how your body absorbs and processes drugs. For example, if you take Synthroid for hypothyroidism, your dose often needs to go up by 25-50% in the first trimester. If you don’t tell them you’re on it, your TSH levels could stay off, affecting your baby’s brain development.
- Are any of your meds interacting with each other? St. John’s Wort cuts the effectiveness of birth control pills by up to 50%. That’s not a myth - it’s in the Pharmacotherapy Journal. And if you’re on an antidepressant and start taking tryptophan supplements, you could risk serotonin syndrome.
- Are you planning to breastfeed? Some meds pass into breast milk. Most are safe, but a few aren’t. Lithium, certain chemotherapy drugs, and some anti-anxiety meds require caution. Your OB/GYN can help you find safer alternatives if needed.
Questions You Should Ask - No Excuses
You’ve got five to ten minutes with your provider. Make them count. Here are the top questions to ask - and why they matter:
- “Is this medication safe during pregnancy?” Don’t settle for “I think so.” Ask if it’s classified as Category A, B, C, D, or X. Category A means proven safe. Category X means avoid - it causes birth defects. Most meds are Category C - meaning animal studies show risk, but human data is limited. That’s okay - your provider can still help you decide if the benefit outweighs the risk.
- “Is there a safer alternative?” If you’re on ibuprofen, ask about acetaminophen. If you’re on a statin for cholesterol, ask if you can switch to diet and exercise for now. There’s almost always a safer option.
- “When should I stop this before trying to conceive?” Some meds, like certain acne treatments or autoimmune drugs, need to clear your system months before pregnancy. Waiting until you’re pregnant to stop them is too late.
- “Will this affect my fertility?” Some blood pressure meds and antidepressants can lower ovulation rates. If you’ve been trying to get pregnant for a while, this is a critical question.
- “What happens if I accidentally took this before knowing I was pregnant?” Panic doesn’t help. Most of the time, the risk is low. But your provider needs to know so they can monitor for signs of complications.
What You Should Never Say - And What to Say Instead
Here are common phrases that shut down good conversations - and how to fix them:
- “It’s just a supplement.” → Say: “I take Nature Made Prenatal and ginger capsules for nausea. Are these okay?”
- “I only take it when I need it.” → Say: “I take ibuprofen for headaches, about twice a month. Should I stop?”
- “My doctor said it was fine.” → Say: “My GP said I could keep taking this, but I want to make sure it’s safe for pregnancy.”
- “I didn’t think it mattered.” → Say: “I didn’t realize this could affect my baby. Can you help me understand what’s safe now?”
Remember: Your OB/GYN has seen this a thousand times. They won’t judge you for being honest. They’ll respect you for being prepared.
What Happens After the Appointment
Good OB/GYNs don’t just give you a list of “yes” or “no” drugs. They give you a plan. You might get:
- A switch from a risky drug to a pregnancy-safe one (like switching from lisinopril to methyldopa for high blood pressure).
- A referral to a maternal-fetal medicine specialist if you’re on multiple high-risk meds.
- A recommendation to start or increase folic acid - at least 400 mcg daily, ideally starting three months before conception. This cuts neural tube defects by up to 70%.
- A follow-up blood test to check if your medication levels are still effective (like TSH for thyroid meds or lithium levels).
If you’re breastfeeding, ask about timing. Some meds are safest if you take them right after nursing, so the baby gets the least amount in the milk. Your provider can help you map out a schedule.

Common Mistakes - And How to Avoid Them
Based on patient feedback and clinic data, here are the top errors - and how to dodge them:
- Mistake: Forgetting herbal teas and supplements. Solution: Write down every bottle in your cabinet. Even “natural” doesn’t mean safe.
- Mistake: Waiting until you’re pregnant to talk about meds. Solution: Start this conversation before you try to conceive. That’s when you have the most options.
- Mistake: Assuming your OB/GYN knows your full history. Solution: Bring a printed list. Or use a free app like MyTherapy or Medisafe to track everything.
- Mistake: Feeling embarrassed about cannabis or alcohol use. Solution: Be honest. The 2022 National Survey on Drug Use and Health found 18% of reproductive-aged women use medical marijuana. Your provider needs to know to monitor for growth issues or withdrawal symptoms in the baby.
When to See a Pharmacist Instead
OB/GYNs are experts in pregnancy - but not always in complex drug interactions. If you’re on four or more medications - say, for diabetes, depression, high blood pressure, and arthritis - your OB/GYN may refer you to a pharmacist who specializes in women’s health. These specialists can review all your meds together, spot hidden interactions, and suggest alternatives you might not have considered. It’s not a sign you’re doing something wrong. It’s a sign you’re being smart.
Final Thought: This Is Your Body. Your Rules.
You’re not just a patient. You’re the person who lives with your body, your meds, your symptoms, and your choices. Your OB/GYN is there to guide you - not to dictate. But they can only do that if you show up with the facts. Take 10 minutes before your appointment. Write it all down. Bring your phone with the photos. Ask the hard questions. You’re not being difficult. You’re being responsible. And in pregnancy, that’s the most powerful thing you can do.
Can I keep taking my antidepressants during pregnancy?
Many antidepressants, including SSRIs like sertraline and citalopram, are considered low-risk during pregnancy and are often continued if they’re helping manage depression. Stopping abruptly can be more harmful than staying on them. Your OB/GYN will work with your mental health provider to choose the safest option and monitor you closely. Never stop cold turkey - always talk to your doctor first.
Is it safe to take ibuprofen while pregnant?
Ibuprofen is generally not recommended after 20 weeks of pregnancy because it can affect fetal kidney development and reduce amniotic fluid. In early pregnancy, occasional use may be okay, but acetaminophen (Tylenol) is the preferred pain reliever. Always check with your OB/GYN before taking any NSAID, even once.
What about CBD oil or medical marijuana?
CBD and THC can cross the placenta and enter breast milk. While research is still limited, studies link cannabis use during pregnancy to lower birth weight and potential developmental delays. The American College of Obstetricians and Gynecologists advises against using cannabis during pregnancy or while breastfeeding. If you’re using it for medical reasons, tell your provider - they can help you find safer alternatives.
Do I need to stop my birth control before trying to conceive?
You can stop hormonal birth control (pill, patch, ring) right before trying to conceive. Most women ovulate again within a month. There’s no need to wait three months - that’s an old myth. But if you’re on long-acting methods like an IUD or implant, your provider will help you plan the removal timing. Folic acid should start at least one month before you stop contraception.
What if I forgot to mention a supplement and later found out it’s risky?
Don’t panic. Many supplements - like evening primrose oil or high-dose vitamin A - are only risky in large amounts or late in pregnancy. Tell your OB/GYN as soon as you realize. They’ll assess the risk based on how much you took and when. Most cases are low concern, but it’s important to update your file so future visits are safer.


Darragh McNulty
This is literally the most important post I've read all year 🙌 I took ibuprofen for a headache at 8 weeks and panicked for a week. Now I know it's not a catastrophe but I should've told my OB. Thank you for this.
Cooper Long
The clinical precision of this article is commendable. It underscores the necessity of pharmacovigilance in obstetric care. One must acknowledge the paucity of longitudinal data on maternal medication use, yet the evidence-based framework presented here is exemplary.
Sheldon Bazinga
lol so now im supposed to tell my doc i smoke weed bc my anxiety is wild? like bro i dont wanna get my baby taken. also why does everyone act like st johns wort is some devil potion? my grandma used it for 40 years and i turned out fine lmao
Sandi Moon
Let me guess - this was written by a pharmaceutical lobbyist. The CDC data is cherry-picked, the ‘safe alternatives’ are all patented drugs with undisclosed side effects, and they conveniently omit that 90% of birth defects come from unregulated supplements and environmental toxins. You’re being manipulated into trusting a system that profits from your fear.
Kartik Singhal
Honestly? This is just another western medical dogma. In India, we’ve been using ashwagandha, turmeric, and neem for centuries during pregnancy. No one died. No one had deformed babies. Now you want us to stop because some FDA study says ‘possible risk’? 😒
Logan Romine
So let me get this straight - you’re telling me to bring photos of my medicine cabinet to my OB like I’m auditioning for ‘Hoarding: Pregnancy Edition’? 🤡 I mean… I guess if I want to be a ‘responsible’ adult, but honestly? My doctor just asks if I’m still drinking coffee. That’s it. I’m fine.
Noah Fitzsimmons
Wait, so you’re telling me to tell my doctor I use CBD oil? But what if she judges me? What if she thinks I’m a bad mom? What if she reports me to child services? I mean, I’m not even high, I just use it to sleep. And now I’m supposed to feel guilty for needing to function? I’m exhausted. Why does everything have to be so complicated?
Simone Wood
I dont even know why i bother going to the dr anymore. last time i mentioned i took melatonin for sleep they acted like i was smuggling cocaine. and then my insurance denied my prenatal vitamins because they said 'it's not medically necessary'. like. i'm literally trying to be responsible and the system is just... broken.
Swati Jain
SIS. THIS. 🙏 I used to think herbal teas were ‘natural’ so they were safe. Then I learned red raspberry leaf can trigger contractions. I cried. But now I’m educated. You’re not being paranoid - you’re being proactive. Keep sharing this. We need more of this in our communities.
Florian Moser
This is exactly the kind of information every expecting parent needs. Writing things down, taking photos of bottles, asking for alternatives - these aren’t extra steps. They’re lifelines. You’re not being difficult. You’re being the best advocate your baby will ever have. Keep going.
Donald Frantz
I appreciate the depth of this, but I’m curious - what’s the evidence base for the claim that St. John’s Wort reduces birth control efficacy by 50%? The Pharmacotherapy Journal citation isn’t linked. Can you clarify the study design? Is it in vitro? Retrospective? Controlled trial?
Sammy Williams
I just sent my OB the photo album of my meds. She laughed and said ‘this is the best list I’ve ever seen.’ I felt like a superhero. Also, I stopped taking my fish oil because I thought it was ‘just a supplement.’ Turns out it’s actually important. Thanks for the nudge.
Elaina Cronin
I must express my profound gratitude for the meticulous attention to pharmacological safety outlined herein. The societal normalization of self-medication during gestation is a grave public health concern. One must not underestimate the teratogenic potential of seemingly benign substances. Your diligence is exemplary.
Willie Doherty
I read this and thought: why is no one talking about the fact that OB/GYNs are often undertrained in pharmacology? I had a doctor who didn’t know the difference between sertraline and escitalopram. This article is good, but it shouldn’t be on the patient to fix systemic incompetence.