When you're pregnant or planning to breastfeed, taking any medication-whether it's for depression, high blood pressure, or even a common headache-can feel overwhelming. You’re not just thinking about yourself anymore. You’re weighing risks for your baby too. And yet, too many people are left guessing, scrolling through Reddit threads or asking friends instead of getting clear, evidence-based answers from their provider. This isn’t just about fear. It’s about safety. Every year, thousands of pregnant individuals take medications without fully understanding the risks because no one took the time to talk through it properly.
Why This Conversation Matters More Than You Think
In the U.S., about 90% of pregnant people take at least one medication during pregnancy. Seven out of ten take prescription drugs. That’s not rare. That’s normal. But here’s the problem: 3% of birth defects are linked to medication exposure-and nearly all of them are preventable. The key? Talking early, often, and with the right tools. The old A, B, C, D, X pregnancy risk categories? They’re gone. Since 2015, the FDA switched to a more detailed labeling system that explains risks in plain language: fetal development risks, maternal health benefits, and breastfeeding considerations-all in one place. But if your provider still says, “It’s Category B, so it’s fine,” they’re using outdated info. You need more than a letter. You need context.When to Start the Conversation
Don’t wait until you’re 12 weeks along and already on a medication. Start before you conceive.- Preconception: If you’re trying to get pregnant-or even thinking about it-review all your meds with your doctor or pharmacist. Some drugs, like isotretinoin (for acne) or certain seizure medications, need to be stopped months before conception. Others, like metformin for PCOS or SSRIs for depression, may be safe and even necessary.
- Prenatal visits: Every time you see your OB/GYN or midwife, ask: “Is everything I’m taking still safe?” Don’t assume they remember your list. Bring a written list of all prescriptions, supplements, and OTC meds. Even that herbal tea you think is harmless might not be.
- Postpartum: Breastfeeding changes everything. A drug that was safe in pregnancy might not be safe while nursing. LactMed, a free database from the National Library of Medicine, has data on over 5,000 drugs and their effects on breast milk. Ask your provider to check it with you.
The Four-Step Framework for Safe Discussions
Top clinics use a simple, proven structure. You can use it too.- Assess your current meds. List every pill, patch, injection, or supplement. Include doses and why you take them. Don’t leave anything out-not even melatonin or CBD.
- Review risks using trusted sources. Avoid Google. Use MotherToBaby (1-800-733-4727) or the TERIS database. These are run by scientists, not advertisers. Their advice matches clinical guidelines 98% of the time. Google? Only 43% accurate.
- Discuss alternatives. Is there a non-drug option? For pain, paracetamol (acetaminophen) is the only recommended analgesic in all trimesters. For anxiety, therapy or mindfulness may be as effective as medication-with no fetal exposure. For high blood pressure, some beta-blockers are safer than others. Ask: “What’s the safest option that still works?”
- Document and follow up. Your provider should document your discussion in your chart using ICD-10 codes like Z33.1 or Z34.00. Get a printed fact sheet from MotherToBaby. Schedule a follow-up in 4 weeks if you’re pregnant, or 2 weeks after birth if you’re breastfeeding.

What Providers Should Be Doing (But Often Aren’t)
A 2023 survey of 15,000 patient stories found that the most appreciated providers did three things:- They gave numbers: “The chance of a problem is about 1 in 1,000-not ‘rare’ or ‘maybe.’”
- They talked about what happens if you stop the drug. Untreated depression or asthma can be riskier than the medication.
- They gave you something to take home: a printed page, a QR code to MotherToBaby, or a note for your pharmacist.
What to Do If Your Provider Won’t Talk
If your OB/GYN brushes off your concerns, or your pharmacist gives conflicting advice, here’s what to do:- Ask for a referral to a maternal-fetal medicine specialist. They’re trained in complex medication use during pregnancy.
- Contact MotherToBaby. They offer free, confidential consultations with teratogen specialists. You don’t need a referral.
- Request a dedicated medication review appointment. Many clinics now offer 15-20 minute slots just for this. If yours doesn’t, ask why.
- Bring a trusted friend or partner. Two ears hear more than one.
Special Cases: Mental Health, Chronic Illness, and Polypharmacy
If you’re on antidepressants, antihypertensives, or multiple medications, your risk profile is higher. About 28% of pregnant people have chronic conditions requiring ongoing meds. Stopping them suddenly can cause seizures, preeclampsia, or postpartum depression. For depression: SSRIs like sertraline are among the safest options during pregnancy and breastfeeding. The risk of untreated depression-including preterm birth or low birth weight-is higher than the medication risk. For diabetes: Insulin is safe. Oral meds like metformin are often continued. But sulfonylureas? Avoid them in late pregnancy. For migraines: Triptans are generally avoided. But acetaminophen with caffeine is often fine. Always check LactMed if you’re breastfeeding.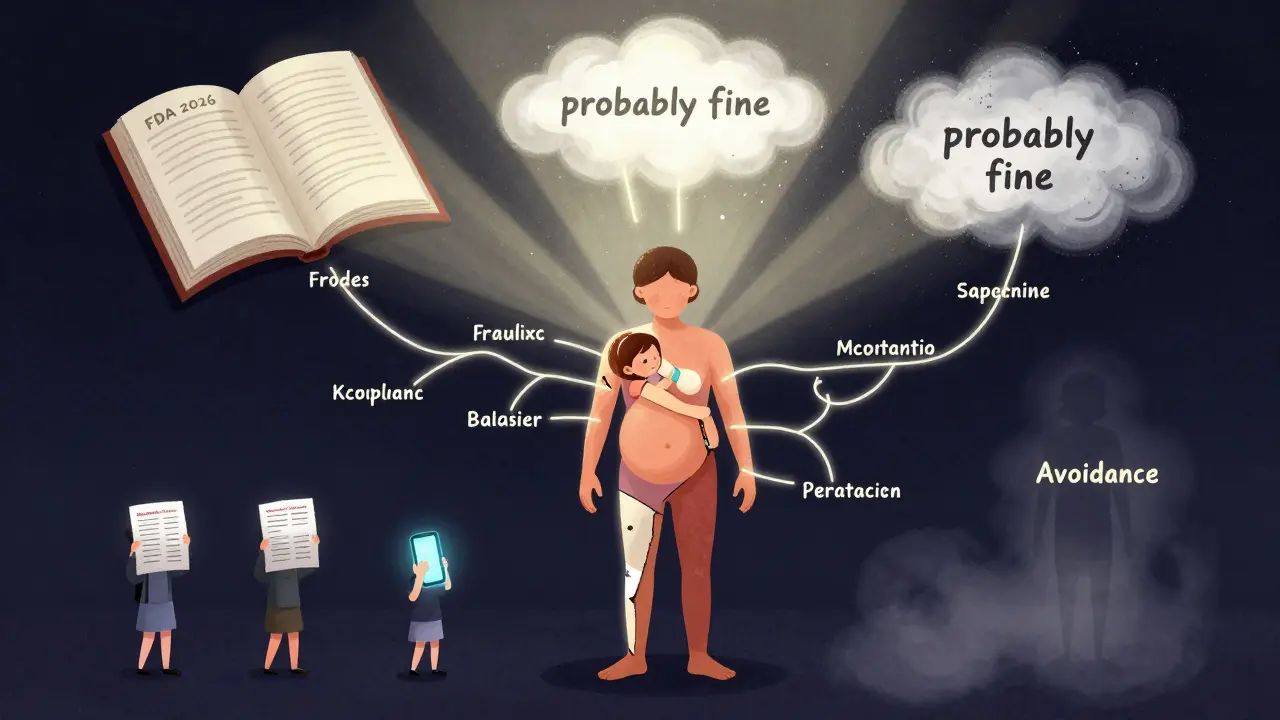
What’s New in 2026
This year, the FDA launched a new initiative requiring all new drug labels to include a clear fetal risk summary. Epic’s EHR system now integrates MotherToBaby’s database directly into its mobile app, so your provider can check a drug’s safety during your visit. Telehealth medication consultations have doubled since 2020. If you live in a rural area without a teratologist nearby, you can now get a video consult with one through your hospital’s telehealth portal. And starting in 2025, all OB/GYN residents in the U.S. will be required to complete training in medication safety communication. That means the next generation of providers will be better prepared.Bottom Line: You Have the Right to Ask
You are not being difficult. You are being responsible. You have the right to know: What does this drug do to my baby? What happens if I don’t take it? Is there a safer option? Can I get this in writing? The data is clear: structured medication safety discussions reduce adverse outcomes by 30%. But only if they happen. Don’t wait for your provider to bring it up. Bring it up yourself. Bring your list. Bring your questions. Bring your fear. And if they don’t have the answers, help them find them-with MotherToBaby, with LactMed, with facts, not guesses.What to Say Next Time
Next time you’re in the office, try this: > “I’m taking [medication name] for [condition]. I want to make sure it’s safe for pregnancy and breastfeeding. Can we go over it using MotherToBaby’s resources? Can you show me the data?” That’s not asking for permission. That’s claiming your right to safe care.Is it safe to take ibuprofen while pregnant?
No. Ibuprofen and other NSAIDs are not recommended after 20 weeks of pregnancy because they can cause low amniotic fluid and heart problems in the baby. Even before 20 weeks, they’re not first-line. Paracetamol (acetaminophen) is the only recommended pain reliever throughout pregnancy. If you’ve taken ibuprofen accidentally, don’t panic-but tell your provider so they can monitor for complications.
Can I keep taking my antidepressants while pregnant or breastfeeding?
Many antidepressants, especially SSRIs like sertraline and citalopram, are considered safe during pregnancy and breastfeeding. The risk of untreated depression-including poor prenatal care, preterm birth, or postpartum complications-is often higher than the medication risk. Never stop abruptly. Work with your provider to find the lowest effective dose and monitor for side effects. LactMed confirms sertraline passes into breast milk in very low amounts, with no reported harm to infants.
What if I’m on multiple medications?
Polypharmacy (taking 5+ medications) affects nearly 3 in 10 pregnant people with chronic conditions. Each drug adds complexity. Ask for a medication review with a clinical pharmacist who specializes in pregnancy. They can identify interactions, suggest safer alternatives, and help you taper off unnecessary drugs. Tools like Lexicomp’s OB/GYN Toolkit and LactMed help prioritize what’s essential.
Are herbal supplements safe during pregnancy?
Most haven’t been studied for safety in pregnancy. Ginger is generally okay for nausea. But herbs like black cohosh, goldenseal, or dong quai can cause contractions or harm fetal development. Always tell your provider about every supplement-even if they don’t ask. Many assume “natural” means safe. It doesn’t.
How do I know if my provider is using up-to-date guidelines?
Ask them directly: “Are you using the FDA’s Pregnancy and Lactation Labeling Rule and checking MotherToBaby or LactMed?” If they say “I’ve always done it this way,” that’s a red flag. Providers using current standards will reference specific databases, show you printed fact sheets, and document discussions in your chart. If they can’t, request a referral to a maternal-fetal medicine specialist or contact MotherToBaby for a second opinion.


jefferson fernandes
Let me just say this: if your provider still uses A-B-C-D-X categories, fire them. Seriously. I’ve seen OBs in 2024 still saying ‘Category B, so it’s fine’-like that’s a medical license to ignore context. The FDA changed the system for a reason: because ‘B’ could mean ‘safe in rats but risky in humans’ or ‘no data but probably okay.’ You need specifics. MotherToBaby isn’t a luxury-it’s your right. And if your provider won’t use it? Print out the fact sheet yourself and hand it to them. They’ll either thank you… or you’ll find someone who will.
Lance Nickie
ibuprofen bad after 20 wks. paracetamol good. done.
Milla Masliy
I’m a doula and I see this all the time-women terrified to ask because they don’t want to seem ‘difficult.’ But here’s the truth: the most empowered people I’ve worked with? They walked in with a printed list of meds, a printout from MotherToBaby, and a calm voice. They didn’t beg. They didn’t argue. They just said, ‘Can we go over this together?’ And guess what? Most providers lit up. They’d been waiting for someone to actually care enough to show up prepared. You’re not being annoying. You’re being the patient they wish everyone was.
John Pope
Oh, here we go again-the ‘structured framework’ cult. Let me break this down for you, because the real issue isn’t the lack of guidelines-it’s the collapse of the therapeutic relationship. You’re being told to ‘bring a list,’ ‘use MotherToBaby,’ ‘document with ICD-10 codes’-as if pregnancy is a compliance audit and not a biological, emotional, spiritual metamorphosis. Where’s the empathy? Where’s the trust? Where’s the recognition that a woman isn’t a pharmacokinetic equation? We’ve turned prenatal care into a checklist-driven dystopia where the only thing more dangerous than the meds is the system that tells you how to ask about them. And now we’re supposed to be grateful because Epic integrated LactMed? That’s like handing a drowning person a life jacket made of spreadsheets.
Don’t get me wrong-I’m not anti-evidence. I’m anti-reductionism. The real risk isn’t ibuprofen. It’s the belief that safety can be quantified, categorized, and delivered via a QR code. You want to know what’s safe? Ask the woman. Listen to her fear. Hold space for her grief if she has to switch meds. That’s medicine. The rest? It’s administrative theater.
Clay .Haeber
Oh wow. So now we’re all supposed to be little pharmacists? Bring your list. Check LactMed. Ask for a ‘medication review appointment.’ Next you’ll be required to pass a quiz on teratogenicity before getting a pregnancy test. I mean, I get it-nobody wants a baby born with flippers. But let’s not pretend this is ‘safe care’ when half the providers still think ‘natural’ means ‘safe’ and the other half think ‘any drug is a death sentence.’ The real problem? We’ve turned pregnancy into a liability lawsuit waiting to happen. And now we’re scaring women into becoming their own clinical pharmacists because the system won’t do it for them. Congrats. We’ve created a world where the only way to not be a bad mom is to read a 50-page FDA whitepaper before breakfast.
Adam Vella
While the article presents a commendable framework for medication safety during pregnancy and lactation, it is critically incomplete in its omission of the epistemological foundations of clinical decision-making under uncertainty. The reliance on MotherToBaby and LactMed, while empirically superior to consumer-driven search engines, still operates within a probabilistic paradigm that does not account for individual genetic variability, epigenetic modulation, or the nonlinear pharmacodynamic responses inherent in gestational physiology. Furthermore, the assertion that ‘3% of birth defects are linked to medication exposure’ is misleading without contextualizing the baseline population risk of congenital anomalies (approximately 3–5%), which is often confounded by polypharmacy, maternal comorbidities, and environmental teratogens. The proposed four-step framework, though logically coherent, fails to integrate shared decision-making models validated in the literature (e.g., OPTION scale), thereby reducing patient autonomy to a transactional checklist rather than a dialogic process. Until the medical community acknowledges that safety is not merely a function of pharmacological classification but of relational trust, patient literacy, and systemic accessibility, these interventions will remain technocratic Band-Aids on a systemic wound.
Nelly Oruko
you dont need to be a doctor to know that if you take something for your anxiety, and you stop it cold turkey? you might not be able to take care of your baby at all. the risk of untreated depression is way higher than the meds. i know. i lived it. dont let anyone make you feel bad for needing help.
Angel Molano
Stop taking everything. Just stop. If you’re pregnant, you’re not a pharmacy. Your body is a temple. If you need drugs to function, you’re doing life wrong. Depression? Pray. High blood pressure? Eat kale. Herbal tea? Drink water. If your body can’t handle motherhood without chemicals, maybe you shouldn’t be a mom. This is the modern disease-thinking you’re entitled to convenience over consequence.
Vinaypriy Wane
I’m from India, and in my village, women take ayurvedic herbs during pregnancy-ashwagandha, shatavari-and no one has ever had a problem. But here, everyone’s scared of everything. I get that science matters. But why is it that in the U.S., a simple ginger tea is treated like poison, while in my country, we use herbs that have been used for 5,000 years? Maybe we need to stop treating pregnancy like a lab experiment and start listening to wisdom that doesn’t come from a database. I’m not saying ignore science. I’m saying: don’t throw out tradition with the bathwater. And please, for the love of God, stop telling women they’re ‘not being responsible’ if they don’t have a 12-page medication log. We’re not robots.