Every year, hundreds of thousands of people end up in hospitals not because their illness got worse, but because the medicine meant to help them made things worse. These are called adverse drug reactions-unexpected, harmful side effects that can range from a nasty rash to organ failure or even death. For many, it’s not bad luck. It’s in their genes.
Why Some People React Badly to Common Medications
Not everyone processes drugs the same way. Two people taking the same pill, at the same dose, can have completely different outcomes. One feels better. The other ends up in the ER. The difference? Genetics. Your DNA holds instructions for enzymes that break down medications. Some people have gene variants that make these enzymes work too fast, too slow, or not at all. Take clopidogrel, a common blood thinner. About 30% of people have a variant in the CYP2C19 gene that stops the drug from activating properly. They’re still taking the pill, but it’s not working. That means they’re at higher risk of a heart attack or stroke-not because the drug failed, but because their body couldn’t use it. Or consider carbamazepine, used for epilepsy and nerve pain. In people of Asian descent, a specific gene variant called HLA-B*1502 can trigger a life-threatening skin reaction called Stevens-Johnson syndrome. Before testing became standard, dozens of cases were reported each year. Now, with a simple blood test before prescribing, that risk drops by 95%. These aren’t rare exceptions. They’re predictable patterns hidden in our DNA.What Pharmacogenetic Testing Actually Does
Pharmacogenetic testing looks at specific genes that affect how your body handles drugs. It doesn’t predict if you’ll get cancer or diabetes. It tells your doctor: “This person metabolizes this drug slowly. Give them half the dose.” Or: “Don’t give this drug at all-here’s a safer alternative.” The most common genes tested include:- CYP2D6 - affects over 25% of all prescription drugs, including antidepressants, painkillers like codeine, and beta-blockers.
- CYP2C19 - critical for clopidogrel, proton pump inhibitors, and some anti-seizure meds.
- TPMT - tells you if you’re at risk of severe bone marrow damage from azathioprine or mercaptopurine (used in cancer and autoimmune diseases).
- SLCO1B1 - predicts statin muscle damage. A simple test can prevent painful, debilitating side effects.
- HLA-B - flags risk for severe skin reactions to carbamazepine, allopurinol, and abacavir.
The Landmark Study That Changed Everything
For years, pharmacogenetics was seen as promising but unproven in real-world settings. That changed in 2023 with the publication of the PREPARE study in The Lancet. This wasn’t a small lab experiment. It was a massive, real-world trial across seven European countries involving nearly 7,000 patients. Before starting any new medication, participants were tested for 50 genetic variants linked to 12 key genes. Their doctors then received alerts in their electronic records suggesting dose changes or alternative drugs. The result? A 30% drop in serious adverse drug reactions compared to the control group. That’s not a small improvement-it’s one of the biggest safety gains in modern medicine. What made this study different? It wasn’t just testing after a reaction happened (reactive testing). It was testing before any drug was given (preemptive testing). And it worked across all kinds of patients-older adults, people with multiple conditions, those on five or more medications. The study proved something doctors had suspected: if you know a patient’s genetic risk ahead of time, you can avoid most of these reactions before they start.How It Compares to Other Approaches
You might wonder: Why not just monitor drug levels in the blood or use clinical risk scores? Therapeutic drug monitoring checks how much of a drug is in your bloodstream after you’ve taken it. But that’s like checking your car’s oil after the engine’s already seized. It doesn’t tell you why it failed. Clinical risk scores use age, weight, kidney function, and other factors to guess your risk. They’re helpful-but they miss the genetic piece. Two people with the same age, weight, and kidney function can have wildly different responses because of their DNA. Pharmacogenetic testing gives you the root cause. It doesn’t guess. It knows. And it’s not just theoretical. In psychiatric care, patients whose treatment was guided by genetic testing saw a 40% reduction in side effects within three months. In cancer clinics, over 100 adverse reactions were prevented per 1,000 patients treated with PGx-guided drugs.
Who’s Getting Tested-and Who Isn’t
Right now, adoption is uneven. Oncology and psychiatry lead the way. In cancer centers, testing for genes like DPYD (before giving 5-FU chemotherapy) is now standard. In psychiatry, testing for CYP2D6 and CYP2C19 helps avoid antidepressants that won’t work-or cause dangerous side effects. But in primary care? Only 18% of clinics use it. Why? Two big reasons: cost and confusion. The test itself costs between $200 and $500. Insurance coverage varies. In the U.S., Medicare covers it for specific high-risk drugs like clopidogrel and thiopurines. In Europe, national health systems are rolling it out more broadly. But even when the test is paid for, many doctors don’t know how to interpret the results. One survey found only 37% of physicians felt confident using pharmacogenetic data. That’s changing fast. Training programs are expanding, and electronic health systems now include built-in alerts. If your doctor sees you’re a “poor metabolizer” of CYP2D6, the system can automatically suggest a different painkiller or lower dose.What’s Holding It Back
The biggest barrier isn’t science. It’s systems. Many clinics still rely on paper records or outdated software that can’t integrate genetic data. Getting test results into the right place at the right time takes time-and money. A full rollout can take 6 to 12 months. There’s also the issue of diversity. Most genetic data comes from people of European descent. That means tests might miss important variants in African, Indigenous, or Asian populations. But that’s changing. The NIH’s Pharmacogenomics Research Network added over 120 new gene-drug links from underrepresented groups in 2024. Another challenge: polypharmacy. If you’re on six medications, and three of them interact with your genes, the advice can get complicated. That’s why clear clinical guidelines-like those from the Clinical Pharmacogenetics Implementation Consortium (CPIC)-are so important. They turn complex data into simple actions: “Avoid this drug,” “Use half the dose,” or “Monitor closely.”What Patients Say
Patients love it. In surveys, 85% say they’d be willing to get tested if their doctor recommended it. They don’t want to be the next statistic. They want to know, before they take a pill, whether it’s safe for them. Some worry about privacy. Can your insurance company use your genetic data against you? In the U.S., GINA (Genetic Information Nondiscrimination Act) protects you from health insurance and employment discrimination based on genetic results. But it doesn’t cover life insurance or long-term care. That’s a real concern for some. Still, most people see the value. One woman in her 60s, after being hospitalized for a bad reaction to a common antidepressant, got tested. Her results showed she was a slow metabolizer of CYP2D6. Her doctor switched her to a different drug. Within weeks, her depression improved-and she stopped feeling sick.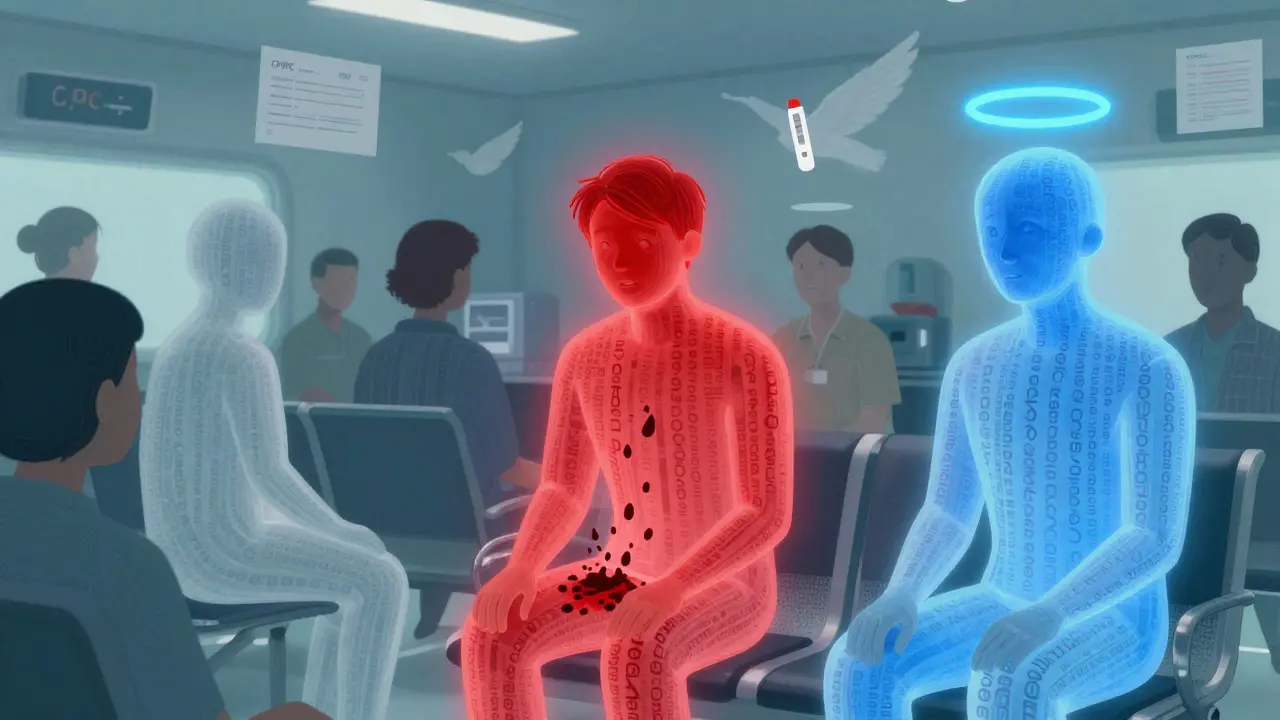
Where This Is Headed
The market for pharmacogenomics is growing fast. It was worth $6.8 billion in 2022. By 2028, it’s expected to hit $22.4 billion. New tech is making testing faster and cheaper. Right now, results take 24 to 72 hours. In the next few years, point-of-care tests could deliver results in under an hour-like a rapid strep test, but for genes. Future versions may combine multiple genes into polygenic risk scores, giving even more precise predictions. Early studies show this can improve accuracy by 40-60% over single-gene tests. By 2026, 87% of major U.S. medical centers plan to offer preemptive pharmacogenetic testing. The European Union is investing €150 million to make it standard across member states. This isn’t science fiction. It’s becoming standard care.What You Can Do Now
If you’ve had a bad reaction to a medication-or if you’re on multiple drugs and feel like something’s always off-ask your doctor about pharmacogenetic testing. You don’t need to wait for a crisis. If you’re about to start:- An antidepressant
- A blood thinner like clopidogrel
- Chemo or chemotherapy-related drugs
- Pain medication like codeine or tramadol
- Statins for cholesterol
- Anti-seizure meds like carbamazepine


Carolyn Benson
So let me get this straight-we’re gonna DNA-test everyone before they take aspirin? Next they’ll be scanning your iris before you buy cough syrup. This isn’t medicine, it’s corporate surveillance with a lab coat. They know your genes, your habits, your debt, your Netflix history-and now they’ll decide what pills you’re ‘allowed’ to take. Welcome to the pharmacological police state. 🤖
Chris porto
I think this is one of those ideas that sounds crazy until you see it work. My uncle took warfarin for years, kept bleeding out for no reason. Got tested-turns out he’s a CYP2C9 poor metabolizer. Switched meds, never had another issue. It’s not magic. It’s just biology finally being respected. Why are we still guessing?
Aadil Munshi
Oh wow, another ‘genetic destiny’ fairy tale. Let me guess-next they’ll tell us our astrological sign determines our metabolism too? 😏 The PREPARE study? Cute. 7,000 people across Europe and you’re acting like this is the Second Coming. Meanwhile, in India, we’ve been adjusting doses based on body weight and liver function since the 80s. No DNA required. Also, who paid for this? Pharma? Because if you’re selling a $500 test to avoid a $20 drug reaction… I smell a profit motive. 🧬💸
Danielle Stewart
If you’re on more than three medications, especially if you’re over 60, please-ask your doctor about pharmacogenetic testing. It’s not a luxury. It’s a safety net. I’ve seen patients go from constant ER visits to stable, feeling like themselves again-just because someone finally looked at their genes instead of their chart. This isn’t futuristic. It’s fundamental. Your body isn’t broken. It’s just not being understood. You deserve better.
jessica .
They want you to get your genes tested so they can track you. That’s how they know who’s ‘high risk’ and who’s ‘low value’. This is how they ration care. You think they care about your health? They care about your insurance premium. GINA? Ha. That law doesn’t cover life insurance. They’ll deny you coverage because your CYP2D6 is ‘slow’. And don’t even get me started on the Chinese gene data they’re buying. This isn’t science. It’s control. 🇺🇸🚫
Ryan van Leent
So instead of telling people to stop mixing alcohol with meds or to tell their doctor about every supplement they take we just give them a $500 test? Sounds like a way to make doctors feel like they’re doing something while avoiding the real issue: people don’t follow instructions. Also why are we testing for HLA-B*1502 but not for ‘stupidity’? That gene’s probably more common
Adrienne Dagg
MY MOM GOT TESTED AFTER HER BAD REACTION TO ANTI-DEPRESSEANTS 😭 SHE’S NOW ON A DRUG THAT ACTUALLY WORKS AND SHE’S SMILING AGAIN 💖 THIS ISN’T JUST SCIENCE-IT’S MAGIC. IF YOU’RE ON MEDS AND FEEL LIKE CRAP, ASK FOR THIS. NO EXCUSES. 🧬✨ #GENETICSWINS
Matt Davies
Imagine a world where your doctor doesn’t have to play Russian roulette with your prescriptions. Where ‘side effects’ aren’t just shrugged off as ‘part of the process’. This isn’t just smart medicine-it’s compassionate medicine. The fact that it’s not standard everywhere is a moral failure. We’ve got the tech. We’ve got the data. Now we just need the will. Let’s make this routine, not revolutionary.