Hepatitis C Eye Health Prevalence Calculator
Eye Condition Prevalence Calculator
Estimate the expected number of hepatitis C patients with specific eye conditions based on clinical prevalence data
Prevalence Results
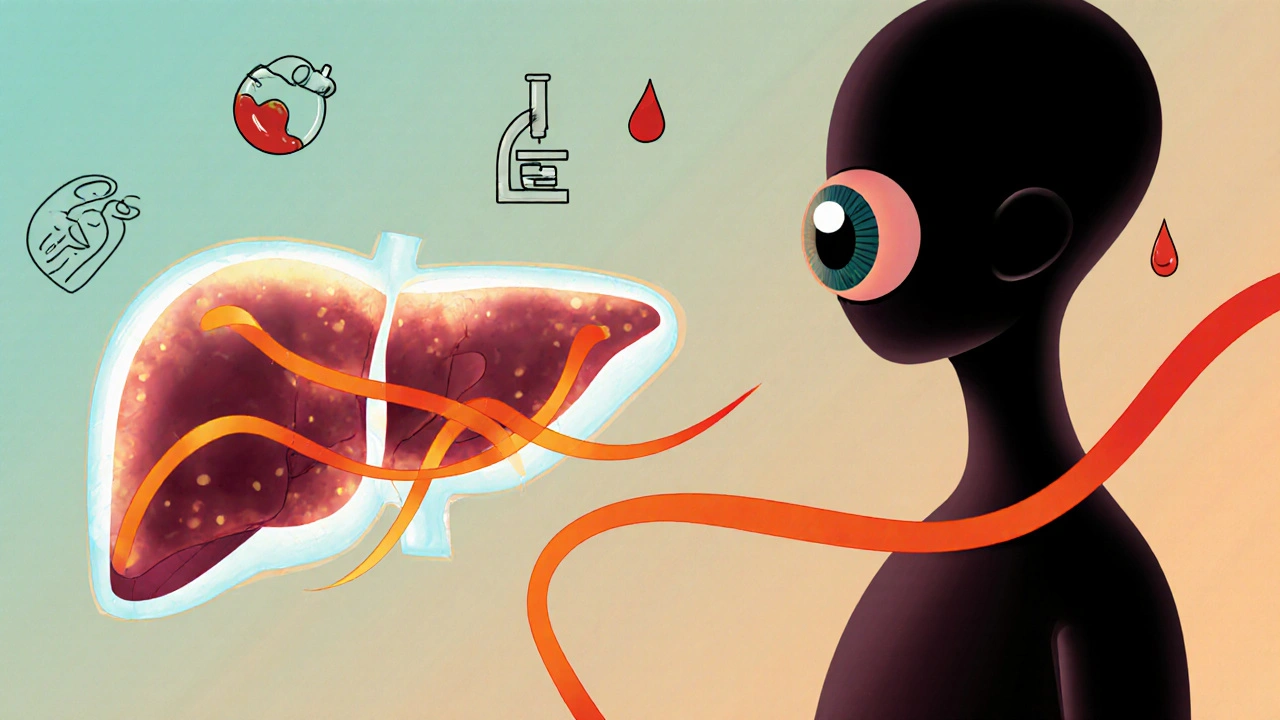
When we talk about Chronic Hepatitis C is a long‑term infection caused by the hepatitis C virus that primarily damages the liver but can affect many other organs, eye health is often overlooked. Many patients assume the virus stays in the liver, yet research shows a clear link between chronic hepatitis C and a range of vision problems.
Why Your Eyes Care About Your Liver
The liver plays a central role in filtering toxins, producing clotting factors, and regulating immunity. When it’s compromised, the entire circulatory system feels the strain. Inflammation becomes systemic, allowing immune complexes and viral particles to circulate to delicate eye tissues. This systemic buzz can irritate the retina, optic nerve, and even the tear film.
Common Ocular Conditions Linked to Chronic Hepatitis C
Below is a snapshot of the eye disorders most frequently reported in hepatitis C patients. The numbers reflect pooled data from several cohort studies up to 2024.
| Eye Condition | Typical Symptoms | Average Prevalence (%) |
|---|---|---|
| Uveitis | Redness, pain, blurred vision | 2‑5 |
| Dry Eye Syndrome | Burning, gritty feeling, intermittent blur | 10‑15 |
| Retinal Vasculitis | Floaters, sudden vision loss | 1‑3 |
| Optic Neuropathy | Color vision loss, visual field defects | 0.5‑2 |
| Cataract | Glare, reduced contrast | 5‑8 |
| Glaucoma | Peripheral vision loss, eye pressure | 1‑2 |
Notice that many of these conditions-especially uveitis and retinal vasculitis-are directly tied to the immune dysregulation caused by the virus.
What Happens Inside the Eye?
Below are the key structures and how the virus can affect them:
- Retina: The light‑sensing layer can suffer from vasculitis, leading to micro‑bleeds and occasional scarring.
- Optic nerve: Inflammation can disrupt signal transmission, causing blurred or dimmed vision.
- Macular degeneration (often age‑related): Chronic inflammation may accelerate the degeneration, especially in patients with existing risk factors.
- Dry eye syndrome: Liver disease reduces tear production and alters tear composition, making the surface gritty.

Screening: Catching Problems Early
Because many eye issues develop silently, regular check‑ups are vital. Here’s a simple schedule for hepatitis C patients:
- Baseline comprehensive eye exam within 6 months of diagnosis.
- Annual dilated retinal exam to watch for vasculitis or macular changes.
- Prompt referral to an ophthalmologist if you notice new symptoms-redness, flashes, or sudden blur.
During the exam, eye doctors will use slit‑lamp microscopy, optical coherence tomography (OCT), and sometimes fluorescein angiography to spot subtle inflammation.
Managing Eye Complications
Treatment often involves two tracks: controlling the hepatitis C virus itself and addressing the specific eye condition.
- Antiviral therapy: Modern Direct‑acting antivirals (DAA) can clear the virus in over 95 % of cases, which dramatically lowers the risk of new eye inflammation.
- Topical steroids or cycloplegics for acute uveitis.
- Artificial tears and omega‑3 supplements for dry eye.
- Laser photocoagulation or intravitreal injections for severe retinal vasculitis.
- Standard glaucoma or cataract surgery when indicated.
Coordinating care between your hepatologist and eye specialist ensures the treatment plan addresses both liver health and vision preservation.
Lifestyle Tips to Protect Your Vision
Even with medication, daily habits play a huge role:
- Stay hydrated: Adequate fluid intake supports tear production.
- Limit alcohol-extra liver strain worsens systemic inflammation.
- Eat a diet rich in leafy greens, carrots, and omega‑3 fatty acids; these nutrients protect retinal cells.
- Avoid smoking; it’s a known risk factor for both liver fibrosis and age‑related macular degeneration.
- Wear UV‑blocking sunglasses outdoors to shield the retina from harmful rays.
When you combine antiviral clearance with these habits, the odds of serious vision loss drop dramatically.
Key Takeaways
- Chronic hepatitis C isn’t limited to the liver; it can trigger inflammation that harms the retina, optic nerve, and tear film.
- Common eye problems include uveitis, dry eye, retinal vasculitis, optic neuropathy, cataract, and glaucoma.
- Annual eye exams and prompt symptom reporting are essential for early detection.
- Effective antiviral therapy (DAAs) reduces the risk of new ocular complications.
- Healthy lifestyle choices-hydration, diet, UV protection, and avoiding alcohol and tobacco-support both liver and eye health.
Frequently Asked Questions
Can hepatitis C cause permanent vision loss?
Yes, if inflammation damages the retina or optic nerve and isn’t treated promptly, permanent loss can occur. Early antiviral treatment and regular eye checks dramatically lower this risk.
What eye symptoms should prompt an immediate doctor visit?
Sudden flashes, new floaters, rapidly worsening blur, eye pain, redness that doesn’t improve, or loss of peripheral vision-all merit urgent evaluation.
Do antivirals fix existing eye damage?
Antivirals halt further viral‑driven inflammation, which can allow some conditions (like dry eye) to improve. However, scarred retinal tissue or cataracts usually need specific ocular treatments.
Is there a link between hepatitis C and glaucoma?
The connection is indirect; systemic inflammation and vascular changes may raise intra‑ocular pressure in susceptible individuals. Regular pressure checks are advisable.
How often should I have my eyes examined if I’m on DAA therapy?
At least once a year during treatment, with a comprehensive dilated exam. If you develop symptoms, see an eye doctor immediately.

Sebastian Green
It's easy to feel overwhelmed when the liver's health seems to spill over into vision problems. The liver's role in filtering toxins really does set the stage for systemic inflammation, which can irritate delicate eye tissues. Regular eye exams, especially a dilated retinal check, can catch early signs before they become painful. Staying hydrated and keeping up with omega‑3 rich foods also helps keep the tear film stable. If you notice any new redness or blurry spots, don't wait – get it checked out.
Andrew Hernandez
The liver‑eye connection is real and often missed. Keeping up with yearly eye checks is a must.
Alex Pegg
Most people think hepatitis C only hurts the liver, but the data shows otherwise. Ignoring the eye risks is just lazy thinking.
laura wood
When you’ve been dealing with chronic illness, the added stress of vision changes can feel isolating. It helps to have a supportive medical team that looks at the whole picture, not just the liver. Keep pushing for those comprehensive eye exams; they’re your best defense.
Demetri Huyler
One cannot simply dismiss the ocular sequelae of hepatitis C as peripheral concerns. The systemic inflammation cascade, catalyzed by viral persistence, orchestrates a subtle yet insidious assault on retinal vasculature. Consequently, the incidence of retinal vasculitis, albeit modest, carries profound visual implications. Moreover, the synergy between antiviral clearance and ocular health underscores the interdisciplinary approach we must champion.
JessicaAnn Sutton
While the mechanistic explanation sounds polished, the moral imperative remains: clinicians must prioritize early detection. Neglecting routine ophthalmic screening violates basic patient care standards. Patients deserve transparent communication about these risks.
jessie cole
Stay strong, folks. Your vision is just another battlefield in the fight against chronic hepatitis C. Make sure you schedule that comprehensive eye exam within six months of diagnosis – it can be a game‑changer. If you notice any new flashes or persistent dryness, reach out to your eye doctor without delay. Together with your hepatologist, you can keep both your liver and your sight in good shape.
Kirsten Youtsey
Don't be fooled by the mainstream narrative that downplays systemic effects. There are hidden networks of influence at play, and the eye is a vulnerable conduit. Vigilance is your only safeguard.
Matthew Hall
Wow, never thought liver disease could mess with your eyes.
Vijaypal Yadav
Statistically, the prevalence of dry eye syndrome in hepatitis C patients hovers around 12 percent, which is notably higher than the general population. This correlation is likely driven by altered tear composition due to hepatic dysfunction. Moreover, retinal vasculitis, though less common, can lead to sudden visual field defects if not identified early. A proactive screening schedule-baseline exam followed by annual dilated checks-significantly reduces the chance of irreversible damage.
Ron Lanham
In the grand tapestry of human health, it is a profound moral failing to overlook the interconnectedness of organ systems. When a virus takes hold of the liver, it does not confine its machinations to that solitary organ; rather, it orchestrates a cascade of systemic inflammation that reverberates throughout the body. The eyes, delicate windows to our perception, are acutely susceptible to such inflammatory assaults. Uveitis, though statistically modest in prevalence, can render a patient’s world hazy and painful, a direct affront to their quality of life. Dry eye syndrome, experienced by a striking ten to fifteen percent of those afflicted, may seem trivial, yet the relentless burning and gritty sensation erodes daily comfort. Retinal vasculitis, with its potential for sudden vision loss, stands as a stark reminder that even rare complications demand vigilance. Optic neuropathy, though affecting as few as half a percent, can irrevocably dim the richness of color and contrast, stripping away the vibrancy of existence. Even cataracts and glaucoma, conditions more commonly associated with aging, acquire an accelerated trajectory under the shadow of chronic hepatitis C. The ethical imperative, therefore, is clear: clinicians must adopt a holistic, interdisciplinary approach that bridges hepatology and ophthalmology. Early detection through regular, comprehensive eye exams is not a luxury but a duty owed to each patient. Antiviral therapy, especially with modern direct‑acting agents, offers a powerful tool to halt further inflammatory damage, yet it does not retroactively heal scarred retinal tissue, underscoring the necessity of prompt intervention. Lifestyle modifications-hydration, nutrition rich in omega‑3 fatty acids, UV protection, and abstention from alcohol and tobacco-serve not merely as adjuncts but as essential pillars of a preventative strategy. In sum, to disregard the ocular sequelae of hepatitis C is to betray a profound responsibility to safeguard the whole person, preserving both sight and the broader tapestry of well‑being.
Mahesh Upadhyay
The moral weight of ignoring eye health is too heavy to bear. Act now, not later.
Rajesh Myadam
I completely understand how daunting all this information can be. Remember that you don’t have to navigate it alone-lean on your healthcare team for guidance. Consistent follow‑ups can catch issues before they become serious, giving you peace of mind.
Kate McKay
Take heart, everyone. Your proactive steps today-hydration, proper diet, regular eye exams-lay the groundwork for a healthier tomorrow. If you ever feel uncertain, reach out to a trusted professional; they’re there to help you stay on track. Keep pushing forward, and don’t let the fear of complications stop you from living fully.