More pregnant women are taking gabapentin or pregabalin today than ever before. In the U.S., about 4 in 100 pregnancies now involve one of these drugs - up from just 2 in 1,000 in 2000. They’re prescribed for chronic pain, nerve damage, anxiety, or epilepsy. But what does that mean for the baby growing inside? This isn’t theoretical. Real babies are being born to mothers who took these medications. And the data, gathered from hundreds of thousands of pregnancies over the last decade, is starting to paint a clearer - and more cautionary - picture.
What Are Gabapentinoids, Anyway?
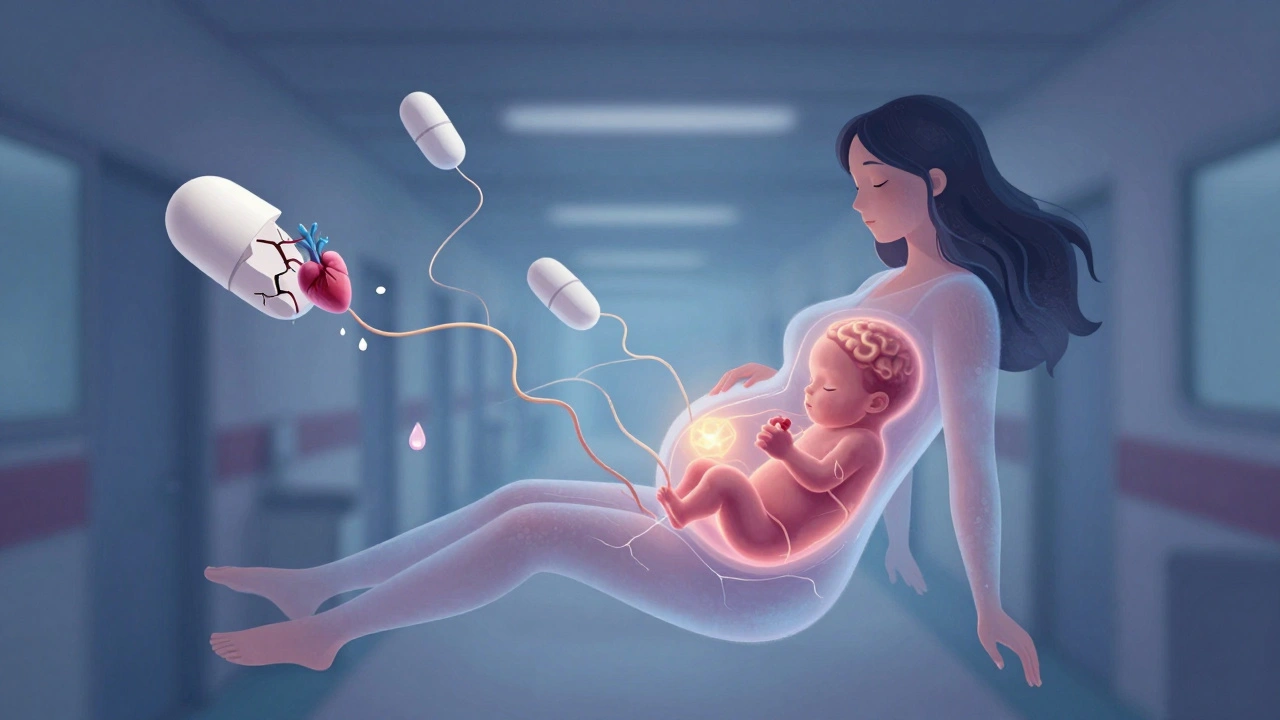
Gabapentin (Neurontin) and pregabalin (Lyrica) are two closely related drugs. They’re not opioids. They’re not traditional antidepressants. They work by calming overactive nerve signals. That’s why they help with pain from shingles, diabetic nerve damage, or fibromyalgia. They’re also used off-label for anxiety and insomnia. But here’s the key point: they cross the placenta. Studies show they reach the baby’s bloodstream and even the brain. That’s not a small detail. It means the developing fetus is exposed to the same drug the mother is taking.
Unlike older seizure meds like valproic acid - which can cause serious birth defects in up to 1 in 10 pregnancies - gabapentinoids don’t seem to cause the same pattern of major malformations. But that doesn’t mean they’re safe. The risks are different, quieter, and harder to spot.
The Big Picture: Major Birth Defects
Early studies raised alarms. Then came the big ones. In 2020, a study published in PLOS Medicine analyzed over 1.7 million pregnancies. It found that gabapentin use during the first trimester was linked to only a tiny increase in major birth defects - 3.2% in exposed babies versus 3% in unexposed. That’s a 7% relative increase, but an absolute risk increase of just 0.2 percentage points. In plain terms: if 100 babies are born to moms who didn’t take gabapentin, about 3 will have a major defect. If 100 babies are born to moms who did, about 3.2 will. That’s not nothing, but it’s not catastrophic either.
But here’s the catch: that number hides a specific danger. The same study found a stronger link to a rare group of heart defects called conotruncal defects. These affect how the heart’s main arteries and chambers form. The risk doubled - from about 0.6 in 1,000 births to 1.2 in 1,000. That’s still rare. But if you’re taking gabapentin daily throughout pregnancy, that risk goes up. And unlike general malformations, this one has a clear pattern tied to consistent use.
Neonatal Problems: The Real Hidden Risk
The biggest concern isn’t what you see at birth. It’s what happens in the first few days after.
A 2018 study in Neurology followed 209 women who took gabapentin until delivery. Of the 61 babies exposed right up to birth, 38% needed to go to the NICU. In the control group - mothers who didn’t take gabapentin - only 3% did. That’s more than a 10-fold difference.
What’s happening? These babies aren’t born with broken hearts or cleft palates. They’re born looking fine. But then they get jittery. They cry nonstop. They can’t feed properly. They have trouble regulating their breathing and temperature. These are signs of neonatal adaptation syndrome - a withdrawal-like reaction. It’s not addiction. It’s the baby’s nervous system suddenly losing a drug it’s been exposed to for months.
Doctors are seeing this more often. And it’s not mild. NICU stays mean separation from mom, feeding tubes, IV fluids, and extra monitoring. For a family already stressed by pregnancy, it’s a heavy burden.

Preterm Birth and Low Birth Weight
It’s not just the baby’s first days. Gabapentin use during pregnancy is linked to higher rates of preterm birth (before 37 weeks) and babies born small for their gestational age. The PLOS Medicine study found a 34% higher chance of preterm delivery and a 22% higher chance of being small for dates. These babies face risks like breathing problems, jaundice, feeding difficulties, and longer hospital stays - even if they don’t have neonatal withdrawal.
Why does this happen? We’re not entirely sure. Gabapentin may affect placental function or maternal hormone levels. It may also be tied to the conditions it’s treating - chronic pain, anxiety, or epilepsy - which themselves can impact pregnancy. But even after adjusting for those factors, the risk remained.
Pregabalin vs. Gabapentin: Is One Safer?
Many assume they’re interchangeable. They’re not.
Pregabalin is more potent, absorbed faster, and stays in the body longer. Animal studies show it causes more developmental harm than gabapentin. The European Medicines Agency says pregabalin should be avoided in pregnancy unless absolutely necessary. In the U.S., both drugs are labeled “Category C” - meaning animal studies showed risk, but human data is limited. But human data is growing - and it’s not reassuring for pregabalin.
Market trends reflect this. By 2027, experts predict pregabalin use in pregnancy will drop by 25-35%. Gabapentin will still be used - but more cautiously. The difference isn’t just in strength. It’s in the weight of evidence.
When Might the Benefits Outweigh the Risks?
This isn’t a blanket “never take it” message. For some women, the alternative is worse.
Imagine a woman with severe, unrelenting nerve pain from spinal surgery. She can’t walk. She can’t sleep. She’s on opioids - and they’re making her nauseated and drowsy. Or a woman with treatment-resistant epilepsy who’s been seizure-free on gabapentin for years. Stopping could mean losing control of seizures, which is far riskier for the baby than the drug.
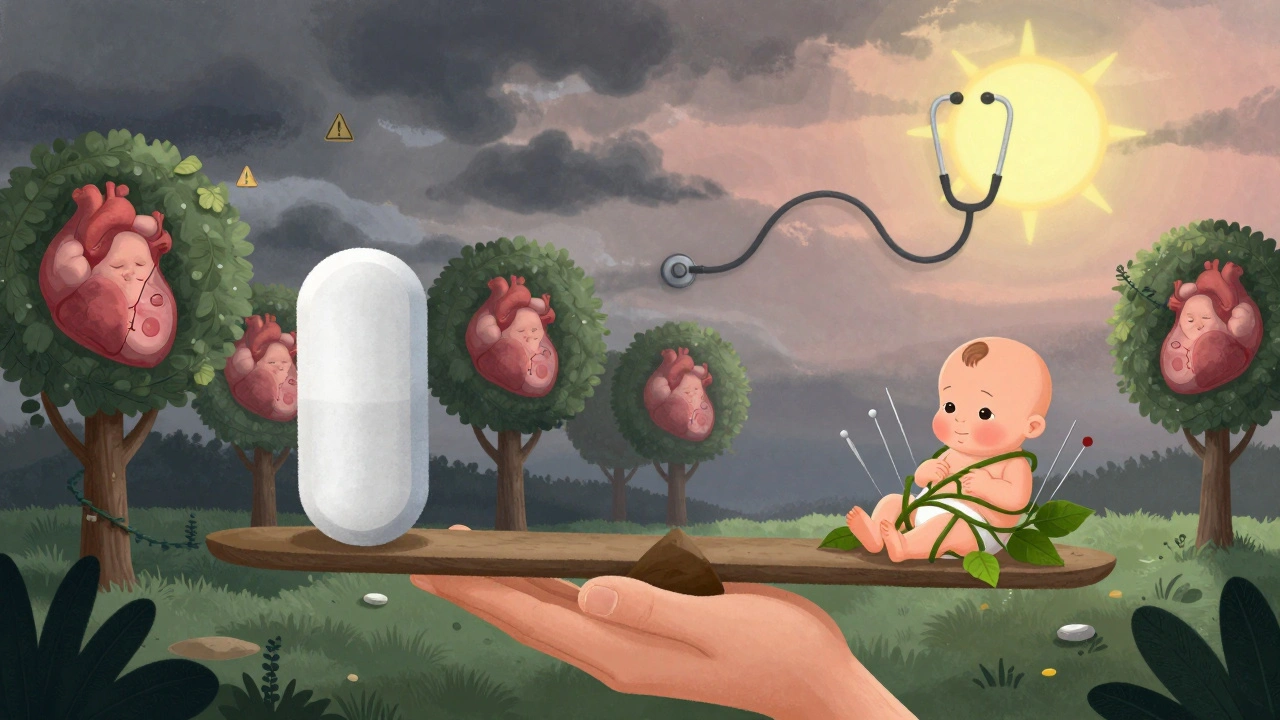
In those cases, doctors may choose to continue. But they don’t do it lightly. The American College of Obstetricians and Gynecologists says gabapentin should only be used when non-drug options have failed and the condition is severe enough to justify the risk. That’s not a casual decision. It’s a careful balancing act.
What Should You Do If You’re Pregnant or Planning to Be?
If you’re taking gabapentin or pregabalin and you’re pregnant - do not stop suddenly. Stopping cold turkey can trigger seizures, severe anxiety, or rebound pain. Talk to your doctor. Together, you can decide whether to taper off, switch to a safer option, or continue with extra monitoring.
If you’re planning a pregnancy and taking one of these drugs, talk to your doctor before you conceive. That’s the best time to adjust. Some women can switch to lamotrigine - an epilepsy drug with a much better safety record in pregnancy. Others may benefit from physical therapy, acupuncture, or cognitive behavioral therapy for pain or anxiety.
And if you’re already pregnant and taking gabapentin? Get a detailed anatomy scan at 20 weeks. Ask for a fetal echocardiogram - a special ultrasound of the baby’s heart. It’s not routine, but if you’ve been on gabapentin regularly, it’s worth it. Catching a heart defect early gives you more options.
The Road Ahead
The FDA just required all gabapentinoid makers to track 5,000 pregnancy outcomes by 2027. That’s a big step. And a long-term study tracking 1,200 children exposed in utero is now underway. We’ll know more about their learning, behavior, and motor skills by 2026.
Right now, the message is simple: gabapentinoids aren’t harmless. They’re not the same as acetaminophen. They’re not even the same as other seizure meds. They carry real, measurable risks - especially if taken late in pregnancy. But they’re also not a death sentence. For some, they’re a lifeline.
The goal isn’t fear. It’s awareness. It’s knowing the trade-offs. It’s making a decision based on facts - not assumptions - and having a plan with your care team.
Is it safe to take gabapentin while pregnant?
Gabapentin is not considered safe for routine use during pregnancy. While the risk of major birth defects is low, it’s linked to higher rates of preterm birth, small babies, and neonatal withdrawal symptoms requiring NICU care. The decision to use it should be made only after careful discussion with your doctor, especially if safer alternatives exist.
Does pregabalin cause more harm than gabapentin in pregnancy?
Yes, current evidence suggests pregabalin carries a higher risk profile than gabapentin during pregnancy. Animal studies show stronger developmental toxicity, and regulatory agencies like the European Medicines Agency advise avoiding it unless absolutely necessary. Experts expect its use in pregnancy to decline significantly in the coming years.
Can gabapentin cause heart defects in babies?
Yes, consistent use of gabapentin during pregnancy - especially throughout all three trimesters - is linked to a small but increased risk of specific heart defects called conotruncal defects. The absolute risk is still low (about 0.8% vs. 0.6% in unexposed pregnancies), but it’s significant enough that doctors now recommend a fetal echocardiogram for women taking it regularly.
What are the signs of neonatal withdrawal from gabapentin?
Babies exposed to gabapentin near delivery may show signs like excessive crying, tremors, irritability, poor feeding, jitteriness, or difficulty regulating breathing and body temperature. These symptoms usually appear within 24-48 hours after birth and may require NICU care. The risk is highest when the drug is taken until delivery.
Should I stop gabapentin if I find out I’m pregnant?
Do not stop gabapentin on your own. Suddenly stopping can cause seizures, worsening pain, or severe anxiety - all of which can harm your pregnancy. Contact your doctor immediately. Together, you can create a safe plan to adjust your medication - whether that means tapering slowly, switching to a safer drug, or continuing with extra monitoring.
Are there safer alternatives to gabapentin for pain or anxiety in pregnancy?
Yes. For nerve pain, physical therapy, acupuncture, or low-dose tricyclic antidepressants like amitriptyline may be options. For anxiety, cognitive behavioral therapy (CBT) is highly effective and safe. For epilepsy, lamotrigine is preferred due to its strong safety record in pregnancy. Always discuss alternatives with your doctor - never assume gabapentin is the only choice.
Final Thoughts
Medication in pregnancy is never black and white. For some women, gabapentin is the difference between functioning and falling apart. But for others, it’s an unnecessary risk. The key is knowing your options, understanding the real data - not the hype - and working with your care team to make the best choice for you and your baby.
There’s no perfect answer. But there is a better way: informed, thoughtful, and individualized care - not a one-size-fits-all rule.

joanne humphreys
I’ve been on gabapentin for fibromyalgia for five years and just found out I’m pregnant. I didn’t realize how much risk was involved, especially with the NICU rates. I’m scheduling an echocardiogram this week and talking to my neurologist about tapering. I’m scared but glad I read this.
Nigel ntini
This is one of the clearest, most balanced summaries I’ve seen on this topic. The distinction between relative and absolute risk is critical-too many people panic over percentages without context. The neonatal adaptation syndrome data is especially alarming, and the emphasis on not stopping abruptly is spot-on. Thank you for highlighting the nuance.
Priya Ranjan
Women today are so careless with medication. Back in my day, we endured pain, we didn’t pop pills and call it motherhood. This isn’t a lifestyle drug-it’s a chemical crutch. If you can’t handle pregnancy without gabapentin, maybe you shouldn’t be pregnant at all.
Gwyneth Agnes
Don’t stop cold turkey. Talk to your doctor. Get the echo.
Ashish Vazirani
Why are we letting Big Pharma dictate what pregnant women take? In India, we’ve managed for centuries with herbs, yoga, and discipline-not chemical Band-Aids! And now Western doctors are normalizing this? It’s a crisis of moral decay wrapped in medical jargon. The baby’s nervous system is not a lab experiment!
Mansi Bansal
It is imperative to underscore that the pharmacokinetic profile of gabapentinoids, particularly their placental transfer and subsequent neonatal exposure, necessitates a paradigm shift in prenatal pharmacotherapy protocols. The conotruncal defect incidence, though statistically marginal, represents a non-negligible teratogenic liability that warrants mandatory fetal echocardiographic surveillance in all exposed gestations. Furthermore, the neonatal adaptation syndrome constitutes a clinically significant iatrogenic entity, requiring multidisciplinary neonatal intervention and parental psychoeducation. The absence of longitudinal neurodevelopmental data remains a critical knowledge gap that must be addressed through prospective cohort studies.
Kay Jolie
Okay but have we talked about the *emotional* toll? Like, imagine being a mom who needs this to function, to not cry all day, to hold her own head up-and then being told she’s a risk? The guilt is real. And the silence around it? Toxic. We need more compassion, not just data points. This isn’t just about birth defects-it’s about mothers who are trying to survive.
pallavi khushwani
I think the real question isn’t whether it’s safe-it’s whether we’re creating a world where women feel like they have to choose between being functional and being a ‘good’ mom. I’ve seen friends taper off gabapentin and spiral into panic attacks that made their pregnancy worse than the drug ever did. Maybe the answer isn’t just ‘avoid’-but ‘support better.’