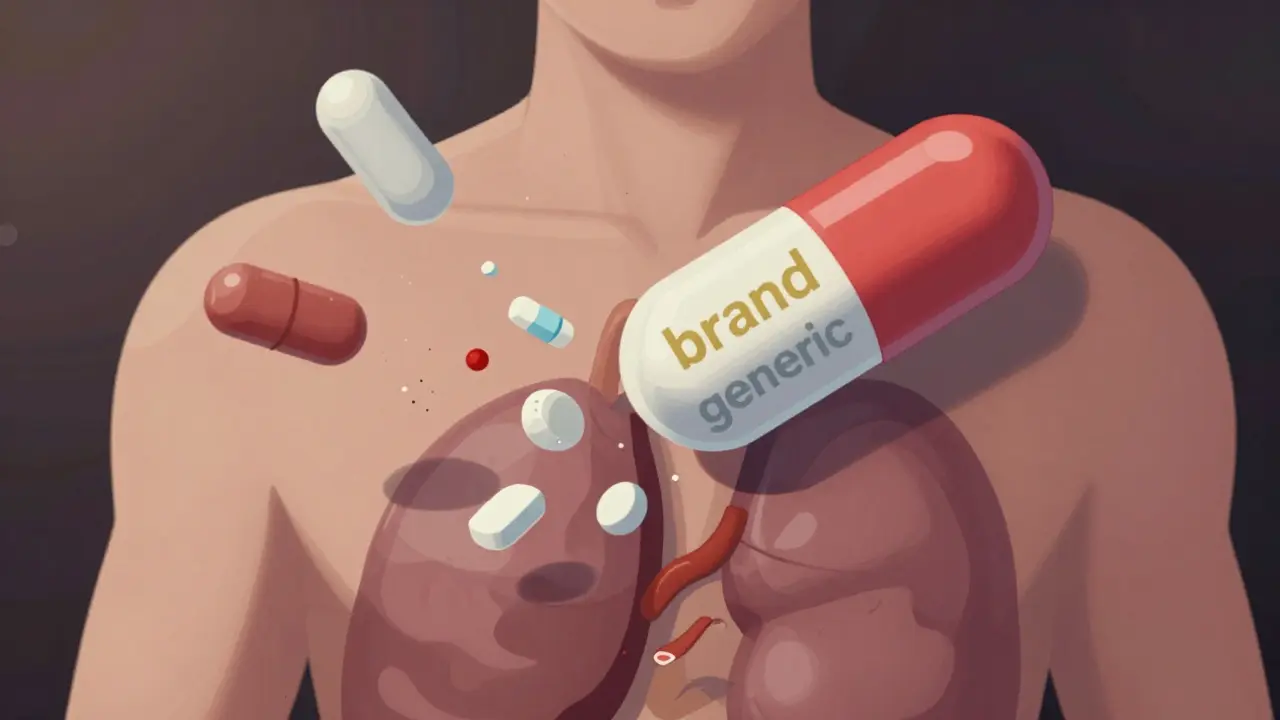
Most people assume that if a generic drug has the same active ingredients as the brand name, it will work the same way. But that’s not always true-especially with combination medications. When you’re taking two or more drugs in one pill, even small differences in the inactive ingredients can throw off how your body absorbs them. And for some patients, that difference isn’t just theoretical-it’s life-changing.
Why Generic Combinations Aren’t Always Identical
Generic drugs are required to contain the same active ingredients in the same strength as the brand version. That part is straightforward. But what’s not required? The fillers, binders, dyes, preservatives, and coatings. These are called inactive ingredients, and they can vary wildly between brands and generics. For most people, this doesn’t matter. But for those on narrow therapeutic index (NTI) drugs, even tiny changes in how the medication dissolves can cause serious problems. Take Advair Diskus, a combination inhaler with fluticasone and salmeterol. A 2021 study found that 23% of patients who switched to a generic version reported using their rescue inhaler more often within 90 days. Why? The generic versions didn’t deliver the same amount of drug to the lungs. The inhaler device itself was different. The powder formulation was slightly altered. The FDA now requires inhaler performance testing for generics of complex devices like this-but it wasn’t always that way. The same issue shows up in oral combinations. Metformin/sitagliptin, used for type 2 diabetes, has multiple generic versions. On Reddit’s r/pharmacy community, users reported stomach upset, bloating, and nausea after switching-symptoms they never had with the brand. The problem wasn’t the active drugs. It was the change in microcrystalline cellulose or magnesium stearate-the fillers used to hold the pill together. For some people, those changes alter how quickly the drug dissolves in the gut.How the FDA Approves Generics (And Where It Falls Short)
The FDA’s standard for approving generics is bioequivalence: the generic must deliver 80-125% of the active ingredient into the bloodstream compared to the brand. This sounds precise, but it’s actually a wide range. Two drugs could be at opposite ends of that range and still be considered “equivalent.” This works fine for most medications. But for drugs like warfarin, levothyroxine, or certain epilepsy medications, even a 5% change in blood levels can mean the difference between control and crisis. A 2020 JAMA study of nearly 90,000 Medicare patients switching from brand to generic levothyroxine found 12.3% needed a dosage adjustment after the switch. That’s more than one in ten. And levothyroxine is a single-ingredient drug. Combination versions? The risk is higher. The FDA’s testing focuses on blood levels over time (AUC and Cmax), but it doesn’t test how the drug behaves in the stomach, how it interacts with food, or how the inactive ingredients affect absorption. A 2017 study found that 47% of generic combination drugs had different inactive ingredients than the brand. That’s almost half. And for patients with allergies-say, to lactose or dyes-that’s not just a footnote. It’s a safety issue.Who’s Most at Risk?
Not everyone needs to worry. But some groups are far more vulnerable:- Elderly patients with multiple prescriptions: Changes in absorption can interact with other drugs, leading to unexpected side effects.
- Patients with chronic conditions like epilepsy, heart failure, or thyroid disease: Their bodies are finely tuned. Small shifts in drug levels can trigger seizures, arrhythmias, or worsening symptoms.
- People with food sensitivities or allergies: Some generics use lactose, gluten, or artificial colors that the brand version avoids.
- Psychiatric patients: A PatientsLikeMe analysis found 31.2% of users reported worsening symptoms after switching generic antidepressants or antipsychotics.

What You Can Do to Protect Yourself
You don’t have to accept whatever generic your pharmacy dispenses. Here’s how to take control:- Check the Orange Book. The FDA’s list of therapeutic equivalence ratings tells you which generics are rated “A” (therapeutically equivalent) and which are “B” (potential concerns). If your drug is on the NTI list, proceed with caution.
- Ask for the brand if you’ve had issues before. Insurance may require prior authorization, but it’s worth it if your health depends on stability.
- Review the inactive ingredients. The pill’s label should list them. If you’re allergic to lactose, soy, or certain dyes, compare the generic to the brand. Many pharmacies now offer this info online or through apps.
- Monitor your symptoms. If you feel different after a switch-more fatigue, mood swings, tremors, or digestive upset-don’t ignore it. Track it. Bring it to your doctor.
- Ask your pharmacist to hold the brand. Many independent pharmacies can order it if you request it. You might pay more, but your health is worth it.
The Bigger Picture: Why This Matters
Generic drugs saved Medicare $1.67 trillion between 2006 and 2019. That’s huge. But the push for cost savings shouldn’t come at the cost of safety. The FDA is slowly catching up. In 2023, they required Teva’s generic Advair to match the brand’s inhaler performance exactly. That’s progress. The Generic Pharmaceutical Alliance has also committed to labeling all inactive ingredients on combination generics by 2025. That’s a step toward transparency. But until then, the burden falls on you and your doctor. There’s no reason to avoid generics entirely. For most people, they’re safe, effective, and affordable. But combination drugs? They’re more complex. And when your health is on the line, you need to know what’s really in that pill.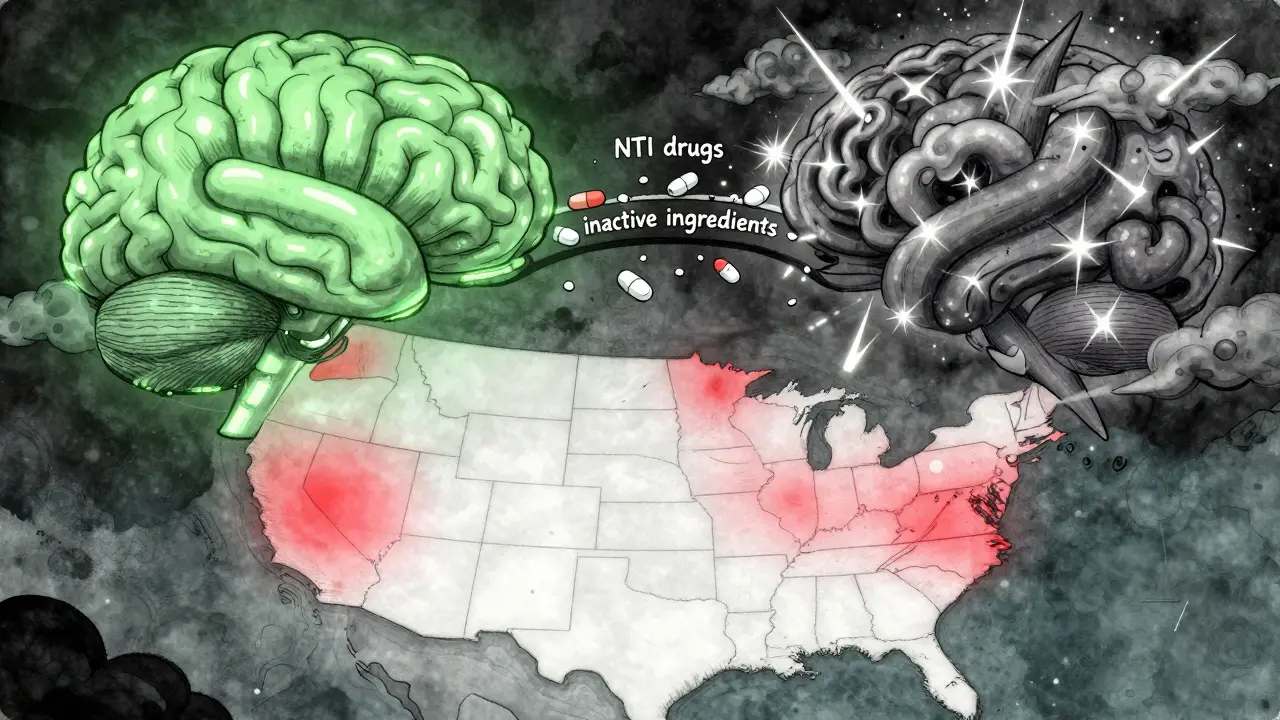
What’s Coming Next
The FDA is rolling out a new system in 2024 to track adverse events linked to formulation differences. The NIH is funding $12.5 million in research to predict which generic formulations might fail in certain patients. And insurance companies are starting to differentiate between standard generics and “authorized generics”-the ones made by the original brand company but sold under a generic label. Authorized generics aren’t cheaper than regular generics. But they’re identical to the brand. For example, Pfizer’s authorized generic version of Lyrica costs 60-70% less than the brand but has the exact same ingredients. If you’ve had trouble with generics before, ask your doctor if this is an option.Final Thought
Medicine isn’t just about molecules. It’s about how those molecules behave in your body. And sometimes, the difference between a brand and a generic isn’t in the active ingredient-it’s in the filler. If you’ve ever felt “off” after a switch, you’re not imagining it. You’re not being difficult. You’re just one of the people for whom the system wasn’t built to account. Don’t be afraid to speak up. Your doctor, your pharmacist, and your insurance company need to hear from you. Because when it comes to your health, the cheapest option isn’t always the best one.Are generic combination drugs always safe?
For most people, yes. Generic combination drugs work just as well as brand-name versions. But for patients on narrow therapeutic index (NTI) drugs-like warfarin, levothyroxine, or certain epilepsy medications-even small changes in inactive ingredients can affect how the drug is absorbed. If you’ve had issues after switching, it’s not in your head. Talk to your doctor.
How do I know if my generic drug has different ingredients?
Check the drug’s labeling, which must list all inactive ingredients. You can also ask your pharmacist for the manufacturer’s product information sheet. Compare it to the brand-name version. If you have allergies to lactose, dyes, or gluten, this is especially important. Some pharmacies now provide this info on their websites or apps.
Can I ask for the brand-name version instead of a generic?
Yes. You have the right to request the brand-name drug. Your insurance may require prior authorization, especially if it’s more expensive. But if you’ve had adverse reactions to generics before, your doctor can write a note explaining why the brand is medically necessary. Many patients with thyroid disease, epilepsy, or psychiatric conditions successfully get this approved.
What’s an authorized generic?
An authorized generic is made by the original brand manufacturer but sold under a generic label. It has the exact same active and inactive ingredients as the brand. For example, Pfizer’s authorized generic for Lyrica is identical to the brand version. It’s cheaper than the brand-usually 60-70% less-but costs 15-20% more than standard generics. If you’ve had problems with other generics, this is often the safest alternative.
Why do some pharmacies automatically switch to generics?
Pharmacies are often incentivized by insurance plans to substitute generics because they’re cheaper. In many states, pharmacists are legally allowed to switch unless the doctor writes “dispense as written” or “no substitution.” But you can always ask them not to switch. If you’ve had bad experiences before, make it clear. Many independent pharmacies will honor your request.
Is there a list of combination drugs that are high-risk for substitution?
Yes. The FDA maintains a list of narrow therapeutic index (NTI) drugs, which includes combinations like levothyroxine/other thyroid agents, certain antiepileptics (e.g., lamotrigine/valproate), and warfarin-based combinations. The 2022 FDA NTI list includes 14 specific drug products. Check the FDA’s Orange Book or ask your pharmacist if your combination drug is on it. If it is, extra caution is needed.

Emma Hooper
Okay but like-why does the FDA even pretend this is okay? I switched to a generic levothyroxine last year and woke up feeling like a zombie who forgot how to breathe. My TSH went from 2.1 to 7.8 in six weeks. My endo said ‘it’s fine, still in range’-but I wasn’t fine. I wasn’t even close. I had to beg for the brand again. They act like we’re all just numbers in a spreadsheet. Meanwhile, my anxiety spiked so bad I started crying in the grocery store aisle. This isn’t science. It’s gambling with people’s lives.
Bennett Ryynanen
Bro. I’m a pharmacist. I’ve seen this. I’ve had patients cry in my aisle because their seizure meds stopped working after a switch. We’re not talking about a headache or a stomach ache-we’re talking about people going back to the ER because a filler changed. The FDA’s 80-125% window? That’s a fucking canyon. I tell every patient with NTI drugs: ‘Don’t let them swap it. Don’t even let them look at it sideways.’ If you’re stable? Stay stable. No one’s gonna thank you for saving $12 a month if you end up in the hospital.
Chandreson Chandreas
Real talk 💯 I had a cousin who switched generics for her epilepsy meds and had a seizure at work. She lost her job. No one believed her when she said it was the pill. Now she only takes the brand-or the authorized generic. It’s not about being ‘difficult.’ It’s about survival. 🙏 The system doesn’t care until you’re in crisis. Don’t wait for that.
Lawver Stanton
Look, I get it. Generics are cheaper. But let’s be real-this whole ‘bioequivalence’ thing is a joke. I’ve had three different generics of metformin/sitagliptin. One made me feel like I swallowed sand. Another gave me migraines. The third? I swear I gained 12 pounds in two weeks just from bloating. And no one in the medical industry wants to hear it. They just say ‘it’s the same active ingredient.’ Yeah, and so is tap water and gasoline, but I wouldn’t drink either. Why are we treating our bodies like lab rats with a coupon? It’s not laziness. It’s negligence wrapped in a cost-saving bow.
Kayla Kliphardt
Do you know where I can find a list of inactive ingredients for my specific generic? My pharmacy’s website doesn’t show it.
Deepika D
Hey Kayla! You can check the FDA’s Orange Book-it has the full inactive ingredient list for every approved generic. Also, most manufacturers have a ‘Drug Facts’ sheet on their website. Just Google the generic name + manufacturer + ‘inactive ingredients.’ If you’re allergic to lactose or dyes, this is non-negotiable. I’ve helped dozens of patients find the right version-sometimes it takes a little digging, but your health? Totally worth it. You got this 💪
Frank SSS
Wow. So we’re just supposed to accept that Big Pharma and the FDA are letting people suffer because someone’s quarterly profit report is looking bad? I mean, I get it-money talks. But when your ‘solution’ to a life-threatening issue is ‘just pay more’-that’s not a fix. That’s exploitation. And the fact that authorized generics exist but are still 15-20% pricier than the regular ones? That’s not capitalism. That’s a rigged game. Someone’s making bank off our desperation.
Darren Pearson
While the anecdotal evidence presented is compelling, it remains insufficient to warrant systemic revision of FDA bioequivalence standards. The aggregate data overwhelmingly supports the therapeutic equivalence of generic medications. To prioritize individual variability over population-level efficacy is to risk undermining the cost-containment mechanisms that have preserved access to essential therapeutics for millions. A more prudent approach would involve enhanced pharmacovigilance and targeted patient education, rather than broad restrictions on substitution.