Eosinophilic esophagitis isn't just heartburn that won’t go away. It’s a chronic immune reaction in your esophagus, triggered by foods your body wrongly sees as invaders. Imagine swallowing a bite of bread or a sip of milk and feeling like it’s stuck, burning, or even choking you. That’s the reality for more than 160,000 people in the U.S. alone, and the numbers are rising fast. Unlike acid reflux, this isn’t about stomach acid-it’s about your immune system flooding your esophagus with eosinophils, a type of white blood cell that’s supposed to fight parasites but ends up tearing up your throat instead.
What Foods Are Really Triggering EoE?
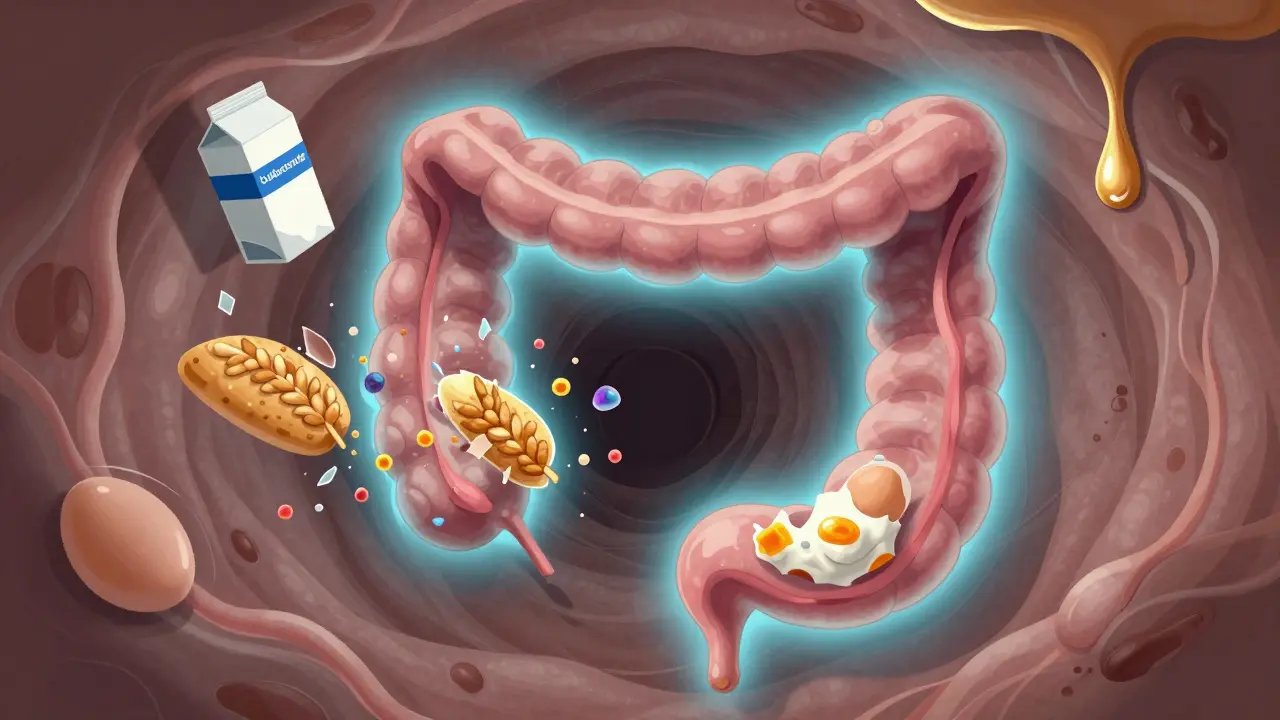
For years, doctors thought you had to cut out six foods to control EoE: milk, eggs, wheat, soy, fish, and nuts. That’s the six-food elimination diet, or 6FED. But here’s the twist: a major 2022 NIH study found that removing just milk alone works almost as well. In adults, eliminating dairy led to remission in 64% of cases. The six-food diet? 65%. No real difference. That’s huge. It means you don’t have to give up everything to feel better.
Why milk? Because it’s the most common trigger. In one study, nearly half of all EoE patients saw their inflammation vanish after ditching dairy-even if they never had a positive allergy test for it. Allergy tests? Skin pricks or blood tests? They’re only right about 20-30% of the time for EoE. That’s why doctors don’t rely on them. The only way to know for sure what’s triggering your symptoms is to remove foods and watch what happens.
But it’s not the same everywhere. In Spain, soy and legumes show up more often as triggers. In the U.S., milk, eggs, and wheat dominate. And kids? They respond even better to the six-food elimination-up to 80% improvement. Adults? More mixed results. That’s why treatment isn’t one-size-fits-all.
How Steroid Slurries Actually Work
If cutting out food sounds overwhelming, there’s another path: steroid slurries. These aren’t inhalers. They’re not meant to be breathed in. They’re swallowed.
Doctors use fluticasone (Flovent) or budesonide (Pulmicort)-medications usually used for asthma-but mix them with water, honey, or applesauce to make a thick paste. You swish it around your mouth, hold it for 30 seconds, then swallow. That way, the steroid coats your esophagus directly, calming the inflammation without flooding your whole body with steroids.
Budesonide oral suspension, branded as Jorveza, got FDA approval in January 2023. It’s specifically made for EoE. In trials, 64% of patients saw their esophagus heal-compared to just 2% on placebo. Fluticasone works too, but slightly less: around 50-60% of people improve. And speed? Most feel better in 2 to 4 weeks. That’s faster than waiting for a diet to work.
But it’s not perfect. About 15% of people get oral thrush-a yeast infection in the mouth. That’s why you have to rinse your mouth after swallowing, even if the slurry tastes awful. One user on Reddit said, “It tastes like chalky mud. I gagged every time. But I did it for 12 weeks… and I could finally swallow my coffee again.”
Why Some People Choose Diet Over Drugs
Why go through the hassle of cutting out entire food groups when steroids work faster? Because drugs don’t fix the root problem. They just quiet the reaction. If you stop taking the slurry, the inflammation comes back. But if you find your trigger food and avoid it, you might never need meds again.
That’s the dream. And for some, it’s real. One patient on HealthUnlocked went from needing esophageal dilation every three months to going 14 months without one-just by cutting out dairy. Another said, “I didn’t know I was allergic to eggs until I ate one after 8 weeks of no eggs. My throat closed up. I knew then.”
But diet is hard. Socially, emotionally, nutritionally. You can’t just grab a burger or a slice of pizza. You have to read every label. You have to plan every meal. And if you’re not careful, you can end up low on calcium, vitamin D, or protein. That’s why working with a dietitian isn’t optional-it’s essential.
There’s also the cost. An elemental diet-where you drink only amino acid-based formulas-can hit $1,800 a month. Most people can’t afford that. But the six-food elimination? It’s free, if you cook at home. And for kids, it’s often the first choice because it avoids long-term steroid use.

What Happens After You Start Treatment?
It’s not enough to just feel better. You need proof your esophagus is healing. That means an endoscopy. Doctors look at the tissue under a microscope and count eosinophils. Remission? Less than 15 per high-power field. That’s the goal.
For steroid slurries, you usually take them for 8 to 12 weeks. Then you get scoped. For diet, you wait 6 to 8 weeks of strict elimination before reintroducing foods one at a time. Each food gets a 2-week trial. If your symptoms return, bingo-you found your trigger.
But here’s the catch: 40% of people who go back to eating their trigger foods see symptoms return within six months. That’s why many stay on low-dose steroids long-term, or stick with a modified diet-like just avoiding milk and eggs.
The New Frontier: Biologics and Better Testing
The future of EoE isn’t just diet or slurries anymore. In May 2023, the FDA approved dupilumab (Dupixent), a biologic drug originally for eczema and asthma. It blocks the specific immune signals driving EoE. In trials, over half of adults reached histological remission. That’s a game-changer. It’s an injection every two weeks. No dieting. No swallowing chalky paste. Just relief.
But it’s expensive. And not everyone qualifies. Right now, it’s usually reserved for people who didn’t respond to diet or steroids. Still, it’s the first treatment that targets the immune system directly, not just the symptoms.
Researchers are also working on better ways to predict triggers without elimination diets. Blood tests for specific proteins in foods, like casein in milk or ovomucoid in eggs, might one day tell you exactly what to avoid. The NIH’s CEGIR study is already testing this. If it works, you could skip months of guessing and start healing right away.
What to Do If You Think You Have EoE
If you’re constantly having trouble swallowing, feeling food stuck, or getting chest pain after meals-especially if you’re young or have other allergies like asthma or eczema-talk to a gastroenterologist. Don’t assume it’s GERD. Ask for an endoscopy with biopsy.
Once diagnosed, work with a team: a GI doctor, an allergist, and a dietitian who knows EoE. Don’t try to DIY this. Start with the simplest option: cut out dairy for 6 weeks. See how you feel. Then talk about steroids if needed. Don’t rush into the six-food elimination unless you’re prepared for the challenge.
And remember: you’re not alone. Groups like APFED and the Eosinophilic Disorders Society offer free resources, meal plans, and even food pantries for people who can’t afford special groceries. There’s help out there.
Real Talk: What Works, What Doesn’t
Let’s cut through the noise.
- Works: Cutting out milk alone for adults. Budesonide slurry. Dupilumab for those who need it. Working with a dietitian.
- Doesn’t work: Relying on allergy tests to find triggers. Stopping steroids too soon. Trying to go it alone without support. Ignoring symptoms because “it’s just heartburn.”
The goal isn’t perfection. It’s control. You don’t have to eat perfectly forever. You just need to know what sets off your body-and how to quiet it down.
Can eosinophilic esophagitis be cured?
There’s no permanent cure yet, but many people achieve long-term remission. For some, avoiding one trigger food like dairy is enough to keep symptoms gone for years. Others need ongoing treatment with steroids or biologics. The key is managing the immune response, not just masking symptoms.
Is a steroid slurry safe for long-term use?
Yes, when used correctly. Topical steroids like budesonide or fluticasone are designed to act locally in the esophagus with minimal absorption into the bloodstream. Side effects like oral thrush are common but manageable with rinsing. Long-term use under medical supervision is considered safe for most patients, especially compared to the risks of uncontrolled inflammation leading to strictures or scarring.
Why don’t allergy tests work for EoE?
EoE isn’t caused by IgE antibodies like typical food allergies. It’s driven by a different immune pathway involving eosinophils and Th2 cytokines. Skin prick and blood tests look for IgE reactions, so they miss the real triggers in most cases. The only reliable way to find triggers is through elimination diets followed by controlled reintroduction.
Can children outgrow eosinophilic esophagitis?
Some children do, especially if their triggers are identified early and avoided. But many don’t. Studies show up to 50% of pediatric patients continue to have symptoms into adulthood. That’s why ongoing monitoring is important-even if symptoms improve, follow-up endoscopies are often recommended to check for hidden inflammation.
What’s the best way to prepare a steroid slurry at home?
For fluticasone, mix 220 mcg (two puffs from a standard inhaler) with 2-3 mL of water or honey. Swirl it gently-don’t shake. Swish in your mouth for 30 seconds, then swallow. Don’t eat or drink for 30 minutes after. For budesonide oral suspension, follow the prescription instructions exactly. Use a syringe to measure the dose. Never use a spoon-it’s not accurate.
If you’re struggling with swallowing, don’t wait. EoE doesn’t get better on its own. But with the right approach-whether it’s cutting out milk, using a slurry, or trying a new biologic-it can be managed. You don’t have to live with food stuck in your throat.

Lauren Scrima
So let me get this straight: I can just ditch dairy and *poof*-no more food stuck in my throat? No more endoscopies? No more chalky mud slurries? I’m crying. Not because I’m sad-because I finally have hope. 🙌
sharon soila
It is truly remarkable how the human body responds to gentle, consistent care. When we remove the triggers that provoke our immune system, we allow it to return to its natural state of balance. This is not merely treatment-it is restoration.
nina nakamura
People still believe in elimination diets like its 2010? The science is clear-dairy isn't the villain. Its the microbiome. You're all missing the point. Fix your gut flora before you cut out milk. And stop taking steroids like they're candy
Hamza Laassili
I dont get why we gotta be so delicate about this?? I mean, if milk makes your throat feel like its full of glue, just dont drink it!! Why do we need a 10-page study to tell us that?? We used to just eat food and not get sick!!
Alvin Montanez
The real tragedy here isn't the eosinophils or the steroid slurries-it's the systemic failure of modern medicine to recognize that chronic inflammation is a symptom, not a disease. We're treating the immune system like a malfunctioning appliance instead of listening to what it's screaming at us. The body doesn't attack harmless proteins out of spite-it's responding to a deeper imbalance, likely environmental, likely nutritional, likely psychological. We keep giving people bandaids while the house burns down.
Lara Tobin
I just started the dairy-free thing last week and already I can swallow my oatmeal without panic 😭 thank you for writing this. I feel less alone now. 💛
Jamie Clark
You're all wasting time. If you're not on dupilumab, you're just delaying the inevitable. The FDA approved it for a reason. This isn't a lifestyle tweak-it's an immunological war. And if you're not fighting with the right weapons, you're just letting your esophagus turn into scar tissue. Get real.
Keasha Trawick
Let’s talk about the *sensory* horror of budesonide slurry. It’s like swallowing a wet chalkboard that’s been dipped in regret and left in the sun. But the miracle? When you finally swallow your first sip of coffee without your throat seizing like a startled cat? Pure. Ecstasy. 🎶✨
Jennifer Taylor
I think the FDA is in on it. They don’t want you to know that dairy is a corporate conspiracy. Big Milk funds the studies. The steroid slurry? That’s just a gateway drug to keep you dependent. I know someone who cured EoE with celery juice and a crystal pendulum. I’m not joking.
Shelby Ume
If you're new to this, please know: you don't have to do this alone. Find a dietitian who specializes in EoE. Join a support group. Even if you're just cutting out milk, you're already doing something powerful. Progress, not perfection. You're doing better than you think.
Jade Hovet
Just did the dairy thing for 6 weeks and my throat feels like a beach vacation 🏖️✨ also I made a dairy-free pizza that didn’t suck. I’m a legend. 🍕❤️
nithin Kuntumadugu
I live in India. We don't even have this problem here. Why? Because we don't drink milk like Americans. We use ghee. And we don't eat bread. This is a Western disease caused by processed food and weak immune systems. Also, I think 5G is involved.
John Fred
Budesonide slurry > diet. No debate. I did both. Slurry worked in 3 weeks. Diet took 8 and I still messed up on a hidden dairy ingredient. Now I just take it twice a day and live my life. No guilt. No labels. Just relief. 🙏
Harriet Wollaston
I used to think I had acid reflux for 10 years. Then I found out I had EoE. I cried in the grocery store because I realized I’d been scared of food my whole life. This post gave me back my appetite. Thank you.