Most people think side effects happen right away. You take a new pill, and maybe you feel dizzy or nauseous the next day. But what if the worst effects don’t show up until you’ve been taking the same medication for years? That’s cumulative drug toxicity - and it’s quietly affecting millions of people on long-term prescriptions.
What Exactly Is Cumulative Drug Toxicity?
Cumulative drug toxicity isn’t about one big reaction. It’s the slow build-up of a drug in your body over time. Think of it like water filling a bucket with a tiny leak. Each dose adds a little more. Your body tries to flush it out, but if the drug leaves slower than it enters, it starts stacking up. Eventually, that bucket overflows - and that’s when symptoms show up.This isn’t rare. About 68% of adverse reactions in older adults taking chronic medications are linked to this slow accumulation, according to the Journal of the National Cancer Institute. Drugs like digoxin, lithium, amiodarone, and even some antibiotics can build up if your liver or kidneys aren’t clearing them fast enough. Fat-soluble drugs - like vitamin A or certain chemotherapy agents - stick around even longer, hiding in fat tissue for months or years.
Why It’s Different From Acute Side Effects
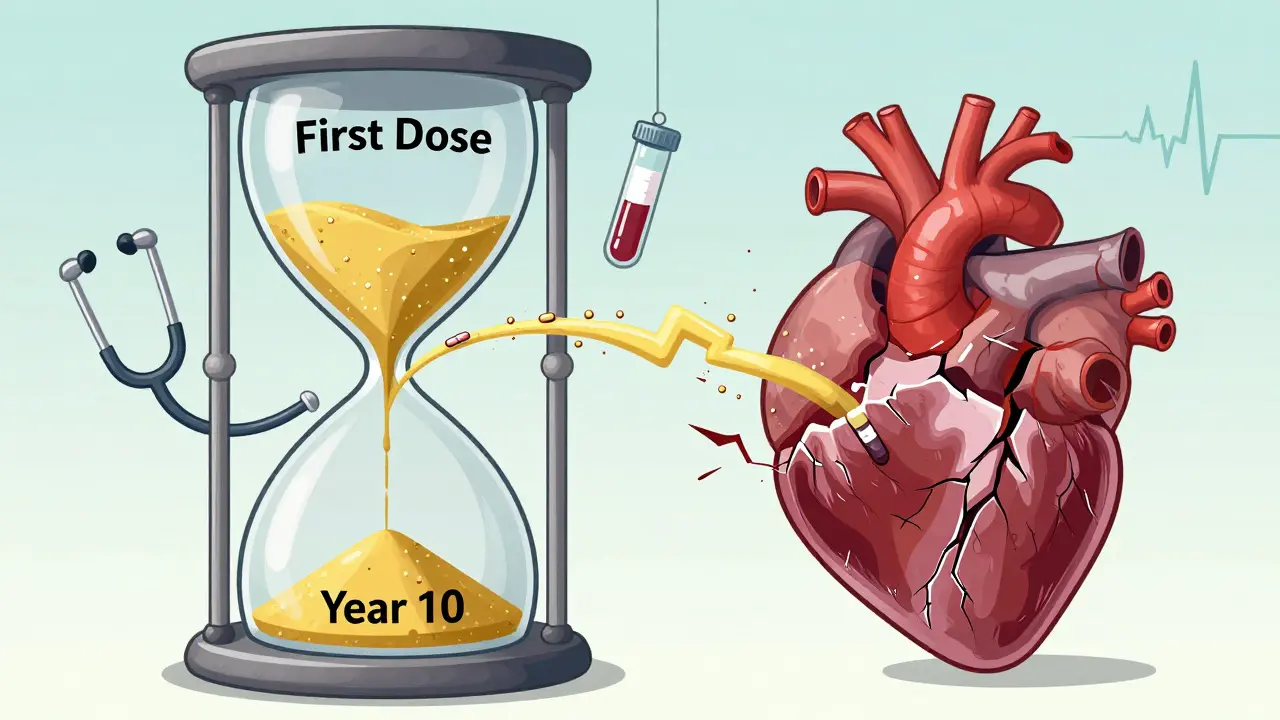
Acute side effects are sudden. You take a dose, you feel bad, you stop. Simple. Cumulative toxicity? It’s sneaky. You might take your blood pressure pill for five years without issue. Then, out of nowhere, you develop heart rhythm problems or liver damage. No sudden spike. No obvious trigger. Just a gradual, silent overload.The difference shows up in the numbers. In cancer treatment, the chance of severe side effects in the first cycle might be around 25%. By the sixth cycle, that jumps to over 50%. The drug hasn’t changed. Your body just can’t keep up anymore. This is why doctors track cumulative doses - especially for drugs like doxorubicin, where exceeding 450 mg/m² can permanently damage the heart.
Who’s at Highest Risk?
Not everyone builds up drugs the same way. Certain factors make you more vulnerable:- Age over 65: Kidney and liver function naturally decline. A 75-year-old might clear a drug 40% slower than a 30-year-old.
- Chronic kidney or liver disease: If your organs are already struggling, even normal doses can become toxic.
- Multiple medications: Drug interactions can slow metabolism. A statin plus a blood thinner? That combo can tip the balance.
- Long-term use: Anticoagulants, antidepressants, thyroid meds, and arthritis drugs are common culprits.
One oncologist on Reddit shared a case where a patient developed severe lung scarring after taking amiodarone for years. Blood tests showed normal levels each time - but the cumulative dose had passed 600 grams. The damage was already done.
Common Medications Linked to Cumulative Toxicity
Here are some drugs you might be on that carry this hidden risk:- Amiodarone: Used for irregular heartbeat. Can cause lung, liver, and thyroid damage after months or years. Lifetime dose limits exist for a reason.
- Digoxin: For heart failure. Narrow therapeutic window. Toxicity can cause nausea, confusion, and fatal arrhythmias.
- Lithium: For bipolar disorder. Requires regular blood tests. Even small increases can lead to tremors, kidney damage, or brain fog.
- Methotrexate: For rheumatoid arthritis and psoriasis. Builds up in the liver. Regular liver scans and folic acid are mandatory.
- Statins: Long-term use linked to muscle damage and, rarely, liver enzyme spikes.
- Antibiotics like aminoglycosides: Can cause permanent hearing loss or kidney damage after repeated courses.
The American Geriatrics Society’s Beers Criteria lists 34 medications with high cumulative risk for seniors. If you’re over 65 and on more than three prescriptions, ask your doctor if any of yours are on that list.
How Doctors Track and Prevent It
The good news? We have tools to catch this before it’s too late.Therapeutic Drug Monitoring (TDM) is the gold standard. Blood tests check how much drug is in your system. This isn’t just for cancer drugs - it’s routine for lithium, digoxin, and vancomycin. But here’s the catch: TDM only tells you the current level. It doesn’t always show the total you’ve built up over years.
That’s why cumulative dose tracking is becoming critical. Some hospitals now use digital systems that automatically add up every pill you’ve taken since you started. One rheumatology clinic reduced methotrexate-related hospital visits by 37% just by implementing this.
Pharmacists are stepping up too. Pharmacist-led programs that review all your meds and calculate cumulative exposure cut hospital admissions for drug toxicity by 29% across 45 healthcare systems.
What You Can Do
You’re not powerless. Here’s what to ask for:- Ask for your cumulative dose history. “How much of this drug have I taken in total?” Most doctors don’t track it - but they can start.
- Request regular blood tests. Especially if you’re on digoxin, lithium, or methotrexate. Don’t wait for symptoms.
- Review all your meds yearly. Bring a list to your doctor - including supplements and OTC painkillers. Some combinations are silent killers.
- Know your kidney and liver function. Get a basic blood panel (creatinine, eGFR, ALT, AST) at least once a year if you’re on long-term meds.
- Don’t skip follow-ups. A Medscape survey found 82% of cumulative toxicity cases involved patients who missed monitoring appointments.
One nurse on AllNurses wrote about patients who’d been on the same antidepressant for a decade. They’d say, “I’ve never had side effects before.” But now they’re dizzy, confused, or losing balance. “They don’t connect the dots,” she said. “They think the medicine is still ‘working fine.’”
The Bigger Picture
This isn’t just a medical issue - it’s a system issue. Only 38% of U.S. electronic health records can automatically track cumulative drug doses. Insurance doesn’t always cover TDM for non-cancer drugs. And drug labels? Many still don’t mention cumulative limits.But things are changing. The European Medicines Agency now requires cumulative toxicity assessments for all new chronic-use drugs. The FDA is using AI to spot patterns in millions of patient records. And the global market for drug monitoring is expected to hit $4.7 billion by 2028.
The bottom line? Long-term medication isn’t harmless. Just because you’ve taken it for years doesn’t mean it’s safe. Toxicity doesn’t announce itself with a bang. It whispers - until it’s too loud to ignore.
Frequently Asked Questions
Can you reverse cumulative drug toxicity?
Sometimes, yes - but not always. If caught early, stopping the drug and supporting organ function (like hydration or liver support) can help. But damage to the heart, lungs, or nerves from long-term buildup is often permanent. That’s why early detection matters more than treatment.
Do over-the-counter drugs cause cumulative toxicity?
Absolutely. Regular use of NSAIDs like ibuprofen or naproxen can cause kidney damage over time, especially in older adults. Acetaminophen (Tylenol) builds up in the liver and can cause failure if taken daily at high doses. Even daily multivitamins with fat-soluble vitamins (A, D, E, K) can accumulate to toxic levels if you’re over-supplementing.
Why don’t doctors always check for cumulative dose?
Many systems don’t track it automatically. Doctors see you once a year and focus on your current symptoms, not your 10-year history. Plus, most medical training still emphasizes acute reactions. But this is changing - especially in oncology, cardiology, and geriatrics. Ask for it. If your doctor doesn’t know how, it’s a sign they need to update their practice.
Are there tests to measure how much drug is in my body over time?
Blood tests show your current level - not your total lifetime exposure. But if you keep records of your prescriptions and doses, your pharmacist can calculate your cumulative amount. Some hospitals now use digital dashboards that auto-calculate this from your e-prescription history. Ask if your clinic has one.
Is cumulative toxicity more common in older people?
Yes, and it’s one of the biggest risks for seniors. Aging reduces kidney and liver function, so drugs stay in the body longer. The Beers Criteria specifically warns against 34 drugs for people over 65 because of this. But it’s not just age - it’s how many drugs you take. Polypharmacy (taking five or more meds) increases risk dramatically.


Candice Hartley
This hit me hard. My grandma was on amiodarone for 8 years and no one ever told us about the buildup. She just got really tired and confused - we thought it was aging. 😔
Andrew Clausen
There is no such thing as 'cumulative toxicity' in the way this article implies. The body metabolizes drugs. If they accumulate, it's because of organ failure or poor dosing - not some mystical slow leak. Stop fearmongering with water bucket analogies.
April Williams
People like you are why we have a healthcare crisis. You take meds like candy and then act shocked when your liver gives out. You think doctors are your personal pharmacists? Wake up. You’re not special. You’re just lazy. 💀
Harry Henderson
STOP SITTING THERE AND TAKING PILLS LIKE THEY’RE CANDY. GET YOUR LABS DONE. ASK FOR YOUR DOSE HISTORY. IF YOUR DOCTOR CAN’T HELP YOU, FIRE THEM. YOUR LIFE ISN’T A GAME. THIS ISN’T A SUGGESTION - IT’S A SURVIVAL CHECKLIST. DO IT NOW.
suhail ahmed
Man, this is wild - in India we call this 'silent poison' because folks don’t realize their chai-spoon of ibuprofen every day for 10 years is slowly turning their kidneys into gravel. One uncle took 4000 mg of paracetamol daily for 'headaches' - ended up on transplant list. Docs didn’t even ask about OTC stuff. We gotta talk about this more.
Paul Taylor
Look I’ve been on lithium for 14 years and I’ve had my levels checked every 3 months like clockwork but I never thought about the total amount I’ve taken over time like a math problem. I mean yeah I’m 62 now and my creatinine is creeping up but I just figured that’s what happens when you get old. Maybe I should ask my pharmacist to crunch the numbers. Never occurred to me before. Interesting.
Kegan Powell
It’s kind of beautiful in a sad way how our bodies try so hard to keep us going even when we’re asking them to carry more than they should. We treat meds like they’re harmless because they’re prescribed but the truth is every pill is a conversation between your cells and a chemical. And if you keep having that conversation for decades without checking in? The cells get tired. And then they stop answering. You’re not broken. You’re just exhausted. 💙
astrid cook
People like Kathy who just shrug and say 'oh I’ve been fine for years' are the reason this problem gets ignored. You don’t get a free pass because you haven’t collapsed yet. Your liver doesn’t care how 'chill' you are. It’s dying quietly and you’re posting memes about it.
Kathy McDaniel
lol i just took a tylenol for my headache and now im paranoid i’m gonna die from liver failure in 2037 🤡
Patrick Merrell
Stop blaming patients. The system is broken. No EHR tracks cumulative doses. Insurance won’t pay for TDM unless you have cancer. Drug labels don’t list lifetime limits. Doctors are overworked and trained on acute care, not chronic monitoring. This isn’t about laziness - it’s about a healthcare system that treats pills like magic bullets and patients like afterthoughts.