Cephalexin vs Alternatives: Antibiotic Selector
Recommended Antibiotic
| Antibiotic | Spectrum | Typical Dose | Pregnancy Category | Cost (AU$) |
|---|---|---|---|---|
| Cephalexin | Gram-positive + limited gram-negative | 250 mg-1 g q6-12h | B | 12-18 |
| Amoxicillin | Broad gram-positive & gram-negative | 500 mg-1 g q8h | B | 8-14 |
| Clindamycin | Anaerobes, MRSA, gram-positive | 300 mg q6h | B | 20-30 |
| Azithromycin | Atypical & some gram-negative | 500 mg daily ×3-5 days | B | 25-35 |
| Dicloxacillin | Penicillin-resistant Staph | 500 mg q6h | B | 10-16 |
| Penicillin VK | Strep, syphilis | 500 mg q6-8h | A | 6-12 |
| Cefadroxil | Similar to Cephalexin | 500 mg q12h | B | 14-20 |
When you hear the name Cephalexin is a first‑generation cephalosporin antibiotic that targets a broad range of gram‑positive bacteria, especially Staphylococcus aureus and Streptococcus species. It’s commonly prescribed for skin infections, ear infections, and urinary‑tract infections. This article gives you a Cephalexin comparison that helps you decide when to stick with it and when another drug might be a better fit.
Key Takeaways
- Cephalexin works best for uncomplicated skin, bone, and urinary infections.
- Amoxicillin offers a broader gram‑negative reach but can trigger more allergies.
- Clindamycin is useful for MRSA‑suspected skin infections but carries a higher risk of C. difficile.
- Azithromycin’s once‑daily dosing is convenient for respiratory issues, yet it’s more expensive.
- Cost, pregnancy safety, and side‑effect profiles often steer the final choice.
What Is Cephalexin?
Cephalexin belongs to the cephalosporin class, introduced in the 1970s. Its mechanism disrupts bacterial cell‑wall synthesis, leading to rapid cell death. Typical adult dosing ranges from 250mg to 1g every 6‑12hours, depending on infection severity. Because it’s excreted unchanged by the kidneys, dose adjustments are needed for renal impairment.
Common Alternatives to Cephalexin
Amoxicillin is a penicillin‑type antibiotic that covers many gram‑negative organisms and is often used for ear, sinus, and dental infections. It’s taken 2‑3 times daily, and its safety profile is well‑known.
Clindamycin targets anaerobes and certain resistant gram‑positive bacteria, making it a go‑to for suspected MRSA skin infections. It’s usually prescribed 300mg every 6hours.
Azithromycin is a macrolide with a long half‑life, allowing once‑daily dosing for 3‑5days, often chosen for respiratory tract infections.
Dicloxacillin is a penicillinase‑resistant penicillin that works well for Staphylococcus aureus skin infections not covered by cephalosporins. Standard dosing is 500mg every 6hours.
Penicillin VK remains a first‑line option for streptococcal pharyngitis and syphilis, with a simple 500mg every 6‑8hours schedule.
Cefadroxil is another first‑generation cephalosporin, similar to Cephalexin but with a slightly longer half‑life, allowing twice‑daily dosing.
How They Stack Up: Comparison Table
| Antibiotic | Spectrum | Typical Adult Dose | Common Side Effects | Pregnancy Category (US) | Approx. Cost (AU$) per Course |
|---|---|---|---|---|---|
| Cephalexin | Gram‑positive + limited gram‑negative | 250mg-1g q6‑12h | Diarrhea, rash, nausea | B | 12‑18 |
| Amoxicillin | Broad gram‑positive & gram‑negative | 500mg-1g q8h | Diarrhea, allergic rash | B | 8‑14 |
| Clindamycin | Anaerobes, MRSA, gram‑positive | 300mg q6h | C.difficile colitis, metallic taste | B | 20‑30 |
| Azithromycin | Atypical & some gram‑negative | 500mg daily ×3‑5days | GI upset, QT prolongation | B | 25‑35 |
| Dicloxacillin | Penicillin‑resistant Staph | 500mg q6h | Hepatic dysfunction, diarrhea | B | 10‑16 |
| Penicillin VK | Strep, syphilis | 500mg q6‑8h | Allergic reactions, GI upset | A | 6‑12 |
| Cefadroxil | Similar to Cephalexin | 500mg q12h | Diarrhea, rash | B | 14‑20 |
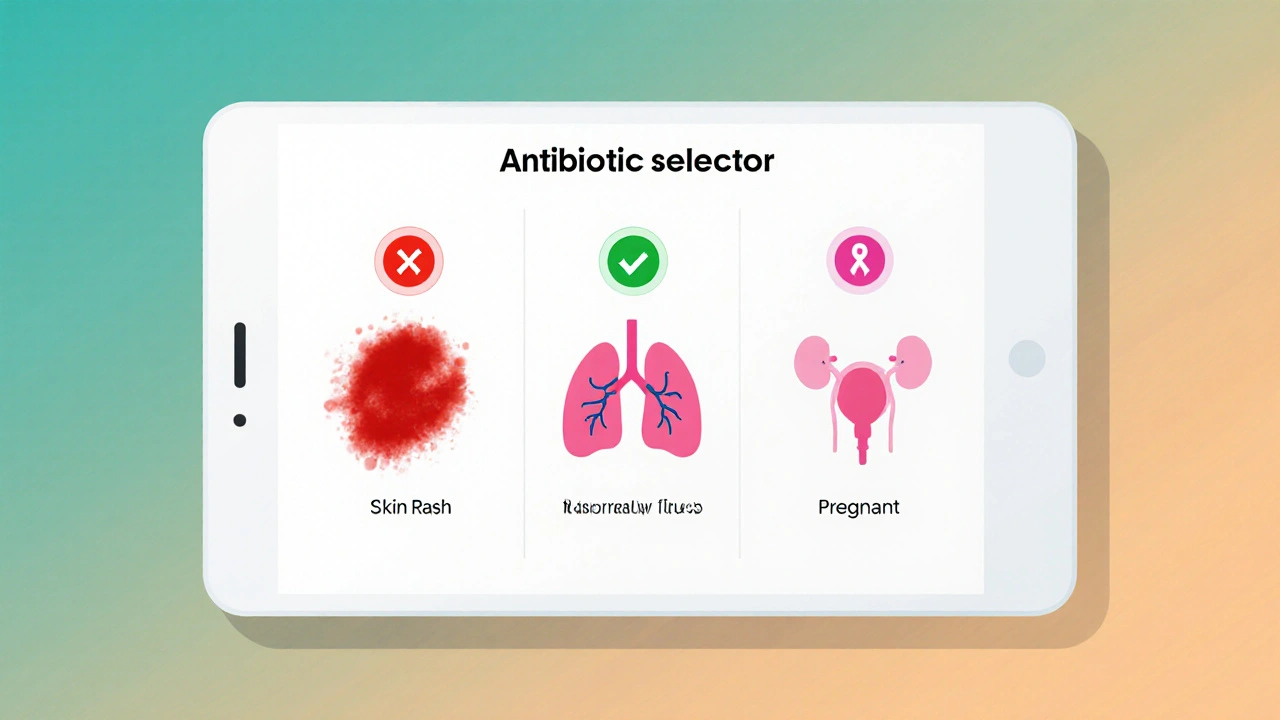
Choosing the Right Antibiotic for Your Condition
For uncomplicated skin infections like impetigo or cellulitis, Cephalexin or Cefadroxil are first‑line because they hit the usual culprits and are cheap. If the infection is suspected to involve MRSA, Clindamycin becomes a safer bet despite its higher cost and C.difficile risk.
Upper‑respiratory complaints (e.g., sinusitis) often respond well to Amoxicillin because it covers Haemophilus and Moraxella. When a patient is allergic to penicillins, Azithromycin provides a macrolide alternative with convenient dosing.
Pregnant patients need a drug in category A or B. Penicillin VK and Cephalexin are both category B, making them the safest choices for skin and urinary infections during pregnancy.
Renal impairment demands dose reduction for drugs cleared unchanged by kidneys (Cephalexin, Amoxicillin, Cefadroxil). For hepatic issues, avoid Clindamycin and high‑dose macrolides.
Safety, Side Effects, and Pregnancy Considerations
All antibiotics can cause GI upset, but the incidence varies. Cephalexin’s mild rash rate sits around 2‑5%, whereas Clindamycin’s C.difficile rate can reach 5‑10% in hospitalized patients. Azithromycin carries a small but real risk of QT prolongation, especially when combined with other cardiac drugs.
Allergy cross‑reactivity is a key factor. Patients allergic to penicillins have about a 10% chance of reacting to cephalosporins like Cephalexin; the risk drops for later‑generation cephalosporins but remains non‑zero.
Pregnancy safety rankings (US FDA) place Penicillin VK in category A (no risk) and most others in B (no evidence of risk). Avoid tetracyclines and fluoroquinolones unless absolutely necessary.
Cost and Availability in 2025
Australian pharmacies list Cephalexin at an average of AU$12‑18 for a 10‑day course, making it the most affordable first‑line option. Amoxicillin sits slightly lower at AU$8‑14, while Clindamycin and Azithromycin can exceed AU$30, reflecting their newer formulations and higher manufacturing costs.
Generic versions of all listed antibiotics are widely available, but supply chain disruptions occasionally affect macrolides. Checking the Pharmaceutical Benefits Scheme (PBS) schedule can confirm subsidy eligibility, which often reduces out‑of‑pocket cost for Cephalexin and Amoxicillin.
Frequently Asked Questions
Can I take Cephalexin if I’m allergic to penicillin?
There is a cross‑reactivity risk of about 5‑10% because both drug families share a beta‑lactam ring. If you’ve had a severe anaphylactic reaction to penicillin, discuss alternatives like Azithromycin with your doctor.
What makes Clindamycin a good choice for MRSA?
Clindamycin’s mechanism bypasses the beta‑lactam resistance pathways that MRSA uses. It achieves high tissue concentrations in skin and bone, which is why clinicians often pick it when MRSA is suspected.
Is it safe to use Azithromycin during pregnancy?
Azithromycin is category B, meaning animal studies have not shown risk and there are no adequate human studies. Many obstetricians prescribe it for respiratory infections when penicillins are unsuitable.
How long does a typical course of Cephalexin last?
Most uncomplicated infections are treated for 7‑10days. Severe skin infections or bone infections may require up to 4weeks, guided by clinical response and lab results.
Which antibiotic is cheapest for a 10‑day skin infection?
Cephalexin typically costs AU$12‑18 for a full 10‑day course, making it the most budget‑friendly option among first‑line agents.


Danielle de Oliveira Rosa
When we contemplate the choice between Cephalexin and its alternatives, it is essential to weigh not only the spectrum of activity but also the patient's individual circumstances, such as renal function, pregnancy status, and potential allergies. Cephalexin offers reliable coverage for gram‑positive organisms and remains affordable, which can be a decisive factor for many patients. However, its limited gram‑negative activity may necessitate a broader agent for mixed infections. In practice, I have observed that clinicians who integrate the patient’s context into the decision‑making process achieve better outcomes and higher satisfaction. Ultimately, the most appropriate antibiotic is the one that aligns with both clinical efficacy and the patient’s unique needs.
Tarun Rajput
In the grand tapestry of antimicrobial stewardship, the decision matrix surrounding Cephalexin versus its phalanx of alternatives demands a nuanced, multilayered appraisal that transcends mere cost considerations and delves deep into pharmacodynamic principles, microbiological spectra, and patient-centric variables. Firstly, one must acknowledge that Cephalexin, as a first‑generation cephalosporin, excels in its capacity to neutralize gram‑positive cocci, particularly Staphylococcus aureus and Streptococcus pyogenes, yet its reach into the gram‑negative domain remains modest, thereby limiting its utility in polymicrobial infections where organisms such as Haemophilus influenzae predominate.
Conversely, Amoxicillin, with its broader gram‑negative coverage, becomes a formidable ally in otitis media and sinusitis, albeit at the expense of a heightened risk of allergic cross‑reactivity in penicillin‑sensitive individuals – a demographic that, while not vast, warrants meticulous screening.
Clindamycin, on the other hand, presents a double‑edged sword: its efficacy against anaerobes and certain MRSA strains is unparalleled, yet the specter of Clostridioides difficile colitis looms large, compelling clinicians to judiciously reserve it for cases with documented or strongly suspected resistant organisms.
Azithromycin introduces the convenience of once‑daily dosing and a propensity to target atypical pathogens, yet its propensity to prolong the QT interval and its comparatively elevated cost impose constraints that must be balanced against patient adherence concerns.
Dicloxacillin, a penicillinase‑resistant penicillin, offers a targeted approach for penicillin‑resistant Staphylococcus, though its hepatic metabolism introduces considerations for patients with liver dysfunction.
Penicillin V remains the gold standard for streptococcal pharyngitis, boasting a Category A pregnancy safety profile, whereas Cefadroxil, akin to Cephalexin but with an extended half‑life, provides dosing convenience without sacrificing antimicrobial potency.
When calibrating the therapeutic regimen, one must also factor in renal clearance; Cephalexin, excreted unchanged in the urine, mandates dosage adjustment in the setting of renal insufficiency, a nuance that can be overlooked in fast‑paced clinical environments.
Moreover, the socioeconomic dimension cannot be ignored: while Cephalexin and Amoxicillin are generally affordable, the financial burden of Clindamycin or Azithromycin may influence prescribing patterns, especially in health systems with limited reimbursement mechanisms.
Pregnancy further complicates the matrix, privileging Category B agents such as Cephalexin and Penicillin V, and dissuading the use of tetracyclines or fluoroquinolones.
In summation, the optimal antibiotic selection is a harmonious synthesis of microbial susceptibility, patient comorbidities, pharmacokinetic considerations, safety profiles, and economic factors, all of which must be meticulously weighed to achieve therapeutic success while minimizing collateral harm.
Joe Evans
Hey folks! 🌟 Cephalexin is great for skin bugs and UTIs, but if you’re allergic to penicillin you might want to look at azithromycin instead. It’s easy to take and works well for a lot of respiratory issues. Just remember to finish the whole course, okay? 👍
Colin Boyd
Honestly Cephalexin is rarely the best choice for anyone
John Petter
While Cephalexin enjoys a reputation for being a workhorse, one must not be seduced by its low price alone. The drug’s spectrum, though adequate for many gram‑positive infections, leaves significant gaps that can jeopardize treatment of mixed flora. In my experience, opting for a broader agent when there is any doubt about gram‑negative involvement prevents therapeutic failure. Nevertheless, the clinical art lies in matching drug to defect, not in blanket prescribing. Therefore, let us reserve Cephalexin for the cases where its strengths truly shine.
Annie Tian
Great overview!; the comparison chart really helps clinicians quickly assess which antibiotic fits best for a given scenario,; especially when considering cost and pregnancy safety,; each option has its own niche,; and it’s reassuring to see clear guidance on dosing adjustments for renal impairment,; keep up the excellent work,; this resource will undoubtedly improve prescribing practices!
April Knof
In many parts of the world, the first‑line antibiotic for skin infections might be a locally available sulfonamide rather than Cephalexin, reflecting regional formularies and cultural prescribing habits. It is fascinating how historical drug availability shapes current practice, and why a global comparison must account for these nuances. Understanding such cultural variations can guide travelers and expatriates in anticipating which medications are most accessible abroad.
Tina Johnson
While the chart is comprehensive, it neglects to address the growing concern of antimicrobial resistance in community settings. The recommendation to default to cheap agents like Cephalexin may inadvertently perpetuate resistance cycles. I would advise integrating stewardship principles more prominently in the decision pathway.
Sharon Cohen
Some might argue that Cephalexin is overused, yet the data still supports its efficacy in uncomplicated cases. I prefer to keep it in the toolbox for straightforward skin infections.
Rebecca Mikell
I appreciate how the post balances clinical detail with readability; it’s a solid foundation for shared decision‑making. Perhaps we could add a short section on patient education for adherence. Overall, a very collaborative effort.
Ellie Hartman
Thinking about how to explain these options to a nervous patient, I find it helpful to compare the side‑effect profiles side by side. Emphasizing that Cephalexin is generally well‑tolerated can reduce anxiety. At the same time, reassuring them about safe choices during pregnancy builds trust. Keep the tone gentle and supportive.
Alyssa Griffiths
It’s worth noting that pharmaceutical lobbying often skews the apparent cost‑effectiveness of drugs like Cephalexin, pushing cheaper generics while obscuring long‑term resistance trends. Moreover, undisclosed data from clinical trials may inflate efficacy numbers; vigilance is essential. Stay skeptical of overly polished presentations.