When you pick up a prescription for a generic pill, you expect it to work exactly like the brand-name version. That’s because small-molecule drugs are made through chemical reactions-like baking a cake from a recipe. Mix the same ingredients in the same order, and you get the same result every time. But biologic drugs? They’re not made that way. They’re grown. Like plants. Or yeast. Or cells in a lab. And that changes everything.
What Makes Biologics So Different?
Biologic drugs are large, complex proteins made inside living cells-often human or animal cells engineered to produce a specific therapeutic protein. Think of them as tiny molecular machines designed to target diseases like rheumatoid arthritis, Crohn’s disease, or certain cancers. Humira, Enbrel, Ozempic-these are all biologics. They’re not chemicals. They’re living products.
These molecules can be up to 1,000 times bigger than a typical pill’s active ingredient. A small-molecule drug like aspirin has about 20 atoms. A monoclonal antibody biologic? It can have over 20,000. And because they’re made by living systems, no two batches are ever exactly alike. Not because of poor manufacturing, but because biology itself is messy. Cells change. Conditions shift. Even tiny differences in temperature, nutrient levels, or pH during growth can alter the final product.
The FDA says it plainly: ‘Slight modifications… are expected as a natural process of manufacturing.’ That’s not a flaw. It’s the rule. And that’s why you can’t just copy a biologic the way you copy a generic drug.
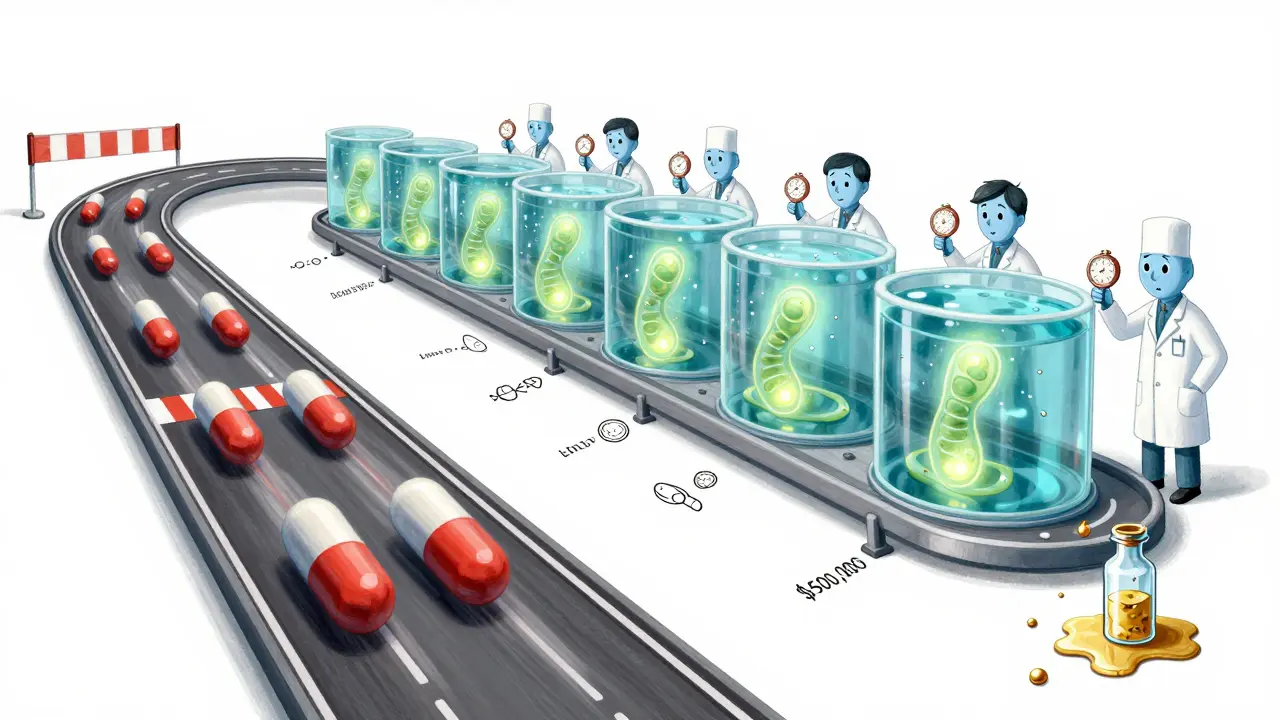
The Manufacturing Process: A 6-Month Marathon
Making a biologic isn’t a factory line. It’s a high-stakes biological ballet. Here’s how it works:
- Cell line development: Scientists insert human genes into host cells-usually Chinese hamster ovary cells-to turn them into protein factories.
- Upstream processing: These cells are grown in massive bioreactors (think 5,000 to 20,000 liters) for 10-14 days. Temperature must stay at 36-37°C. pH must hover around 7.0-7.4. Oxygen levels? Precisely controlled. One dip in cell viability below 95%, and the whole batch could be ruined.
- Downstream processing: After the cells are harvested, the protein must be purified. This involves multiple steps: protein A chromatography (to isolate the target), viral filtration (to remove contaminants), and ultrafiltration. Each step removes impurities but also risks damaging the delicate protein structure.
- Formulation and packaging: The final product is mixed with stabilizers, buffered to the right pH, and filled into vials or pens under sterile conditions.
The whole process takes 3 to 6 months. Compare that to a generic pill, which can be made in days. And the cost? Manufacturing a single batch of a biologic can cost millions. Failure rates? 10-15%. One contaminated tank can wipe out half a million dollars’ worth of product.
Why No One Can Make an Exact Copy
Generics are copies. Simple. Identical. A generic version of ibuprofen has the same chemical structure, the same atoms, the same bonds. It’s a mirror image.
Biologics? Not even close. You can’t reverse-engineer them. You can’t analyze every single atom in a 20,000-atom protein and say, ‘We’ll make this exact thing.’ Current technology can only characterize 60-70% of a biologic’s structure. The rest? Unknown. Unmeasurable. That’s not a gap in science-it’s a fundamental limit of biology.
So instead of copies, we get biosimilars. These are highly similar, but not identical. They must match the original in structure, function, safety, and effectiveness-but they’re allowed to have minor differences. The FDA requires biosimilars to go through years of testing: analytical studies, animal tests, and clinical trials to prove they behave the same way in the body.
And even then, biosimilars aren’t interchangeable by default. Pharmacists can’t swap them in without a doctor’s approval unless they’re designated as ‘interchangeable’-a much stricter standard. Only a handful have met that bar so far.
The Cost of Complexity
Because biologics are so hard to make, they’re expensive. The average biologic costs 10-20 times more than a generic small-molecule drug. But here’s the twist: biosimilars don’t slash prices by 80% like generics do. Why? Because making a biosimilar isn’t cheap either.
Developing a biosimilar takes 7-10 years and $100-$200 million. That’s a fraction of the original biologic’s cost-but still enormous. Companies can’t just buy the formula and start pumping out pills. They have to reverse-engineer a living system. They have to build their own cell lines. Their own bioreactors. Their own purification methods. And even then, they have to prove it’s close enough to the original.
That’s why the biosimilars market, while growing fast, is still small-only $10.5 billion in 2023, compared to $386.8 billion for the original biologics market. The barriers are too high for most companies to enter.

What’s Changing in Biologics Manufacturing?
There’s hope. New technologies are emerging. Single-use bioreactors are cutting contamination risks by 60%. Artificial intelligence is helping predict how small changes in temperature or nutrient mix will affect protein quality. Continuous manufacturing-where the process runs nonstop instead of in batches-is being tested in 15% of new facilities.
But the biggest shift? The industry is moving toward modular, flexible plants. Instead of building massive, fixed factories that cost half a billion dollars, companies are designing smaller, reconfigurable units. Think of it like a kitchen that can switch from baking bread to making pasta just by changing the tools. This could cut capital costs by 25-30% and speed up production.
Still, the core truth remains: biology is not chemistry. You can’t automate away the messiness of living cells. The more we learn, the more we realize that a biologic isn’t just a drug. It’s a product of its process. Change the process, even slightly, and you change the drug.
Why This Matters for Patients
If you’re on a biologic for a chronic condition like psoriasis or multiple sclerosis, you might be wondering: Can I switch to a cheaper biosimilar? The answer is usually yes-but not without your doctor’s input.
Studies show biosimilars are safe and effective. In Europe, where biosimilars have been used for over a decade, there’s no evidence of increased side effects or reduced effectiveness. But because biologics are so complex, some patients report feeling different after switching-even if lab results show no change. That’s why doctors often prefer to keep patients on the same product unless there’s a clear cost or supply benefit.
And for new patients? Biosimilars are opening doors. A biosimilar version of Humira costs about 30-50% less than the original. That’s still expensive-but it’s more affordable than before. And with more biosimilars coming to market, prices will keep dropping.
The bottom line: Biologics aren’t broken because they can’t be copied. They’re just different. And that difference? It’s what makes them powerful. It’s also what makes them so hard to make. But it’s not a flaw. It’s the nature of the medicine.
Can biosimilars be substituted for biologics without a doctor’s approval?
Only if they’re officially designated as ‘interchangeable’ by the FDA. Most biosimilars are not interchangeable. Even if they’re highly similar, pharmacists can’t swap them out automatically. Your doctor must prescribe the specific product, and you should be informed if a switch is made.
Why are biologics so much more expensive than generics?
Biologics require living cells, years of development, and complex, high-precision manufacturing that takes months. A single batch can cost millions. Generics are made from simple chemical formulas that can be replicated quickly and cheaply. The cost difference isn’t about profit-it’s about physics and biology.
Are biosimilars as safe as the original biologics?
Yes. Regulatory agencies require biosimilars to undergo extensive testing-analytical, animal, and clinical-to prove they work the same way. In Europe, where biosimilars have been used for over 10 years, no safety concerns have emerged that weren’t already known from the original drug.
Can I tell if I’m taking a biosimilar instead of the original biologic?
You might not know unless your pharmacy or doctor tells you. Biosimilars have different brand names but similar-looking packaging. Always check the name on the label. If you notice new side effects after switching, tell your doctor-even if it’s minor. Small differences in how your body reacts can matter.
What’s the future of biologics and biosimilars?
More biosimilars are coming. Over 50 are in development for major biologics like Humira and Enbrel. Manufacturing is becoming more efficient with AI and single-use systems. Prices will keep falling-but not as dramatically as with generics. The goal isn’t to copy biologics. It’s to make them more accessible without sacrificing safety or effectiveness.

Swapneel Mehta
Biologics are wild when you think about it. We treat them like machines, but they’re more like living organisms grown in vats. The fact that we can even make them work consistently is a miracle of modern science.
Meina Taiwo
Yep. Biosimilars aren’t generics. They’re like cousins, not twins. And that’s why the testing is so intense.
Jason Silva
So we’re paying $100K/year for a lab-grown protein that’s basically a snowflake? 🤯
Stacey Smith
This is why Big Pharma doesn’t want biosimilars to be interchangeable. Control. Profit. Same old game.
Southern NH Pagan Pride
They’re not letting us copy biologics because they’re hiding something. The FDA’s ‘natural variation’ excuse? That’s corporate speak for ‘we don’t know what’s in it either.’
Adrian Thompson
Let me get this straight - we spend billions to grow a protein in hamster cells, then call it medicine? Meanwhile, China’s making their own version in 18 months with 1/10th the cost. This isn’t science - it’s a cartel.
They call it ‘complexity’ but it’s just a barrier to entry. The same people who made the original drug control the patents, the supply chain, the testing protocols - and now they’re crying ‘it’s too hard to copy!’
Meanwhile, patients are dying because they can’t afford Humira. And we’re supposed to be impressed by the ‘biological ballet’? Nah. This is rent-seeking dressed up as biotech.
Single-use bioreactors? AI? Please. That’s just window dressing. The real innovation would be breaking the patent monopoly. But nope - Congress gets campaign cash from pharma, so we keep paying $70K for a vial of magic.
They say biology is messy? Yeah, but so is capitalism. And guess which one’s easier to fix?
Ben Warren
It is imperative to underscore that the regulatory framework governing biosimilars is predicated upon rigorous analytical comparability, nonclinical evaluation, and clinical demonstration of similarity in pharmacokinetics and pharmacodynamics. To conflate biosimilarity with generic equivalence is to fundamentally misunderstand the ontological distinction between small-molecule pharmaceuticals and macromolecular biologics.
The structural heterogeneity inherent in protein-based therapeutics renders any claim of identity untenable. Even minute variations in glycosylation patterns, folding conformations, or post-translational modifications can alter immunogenicity profiles - a phenomenon that is not merely statistically significant but clinically consequential.
Therefore, the assertion that biosimilars are ‘close enough’ is not merely scientifically inaccurate - it is potentially hazardous to public health. The FDA’s ‘interchangeability’ designation requires not only similarity but also demonstrated clinical equivalence in multiple-switching scenarios - a standard that has been met by fewer than five products in the United States as of 2024.
It is not the fault of the biotechnology industry that biology resists commoditization. It is the responsibility of regulators and legislators to uphold the integrity of therapeutic standards - not to succumb to the siren song of cost reduction at the expense of safety.
Jackie Be
OMG I just realized biologics are basically magic potions grown in giant yeast tanks 😭 I’ve been on one for 5 years and I thought it was just a fancy pill
My doctor switched me to a biosimilar last year and I felt like a ghost for two weeks like my soul got swapped
They should put warning labels like ‘this is alive’
Michael Ochieng
As someone from Kenya, I’ve seen how these drugs are priced out of reach even in wealthy nations. The fact that biosimilars are even slowly becoming available gives me hope. This isn’t just science - it’s justice.
Teya Derksen Friesen
The elegance of biologics lies in their complexity - they are not merely drugs, but living systems engineered to interact with living systems. To reduce them to chemical equivalents is to misunderstand the very nature of biological therapeutics.
Yet, the progress in manufacturing efficiency, particularly through modular platforms and AI-driven process optimization, offers a promising path toward sustainable accessibility without compromising safety.
This is not a failure of science - it is its highest expression.
Hannah Taylor
theyre not letting us copy em because theyre scared someone will figure out the real secret… like the cells are actually sentient and theyre screaming inside the bioreactors
i swear i read a paper once that said the proteins change when you look at them under a microscope
also why do all the biologics have the same logo? coincidence? i think not
John Hay
My cousin’s on a biosimilar for RA and it saved her life. She’s back hiking. The cost dropped from $12K/month to $5K. That’s not a loophole - that’s progress.
Jon Paramore
Key point: glycosylation profiles. That’s the invisible variable. Two biosimilars can have identical amino acid sequences but different sugar attachments - and that changes how the immune system sees them. No commercial lab can fully map that yet. That’s why we need clinical trials - not just chemistry.
Cameron Hoover
It’s beautiful, honestly. We’re not just treating disease - we’re coaxing life itself to heal us. That’s not just medicine. That’s art.
Orlando Marquez Jr
It is noteworthy that the European Medicines Agency has approved over 60 biosimilars since 2006, with no significant increase in adverse events attributable to biosimilar use. This empirical evidence should inform regulatory policy in other jurisdictions.