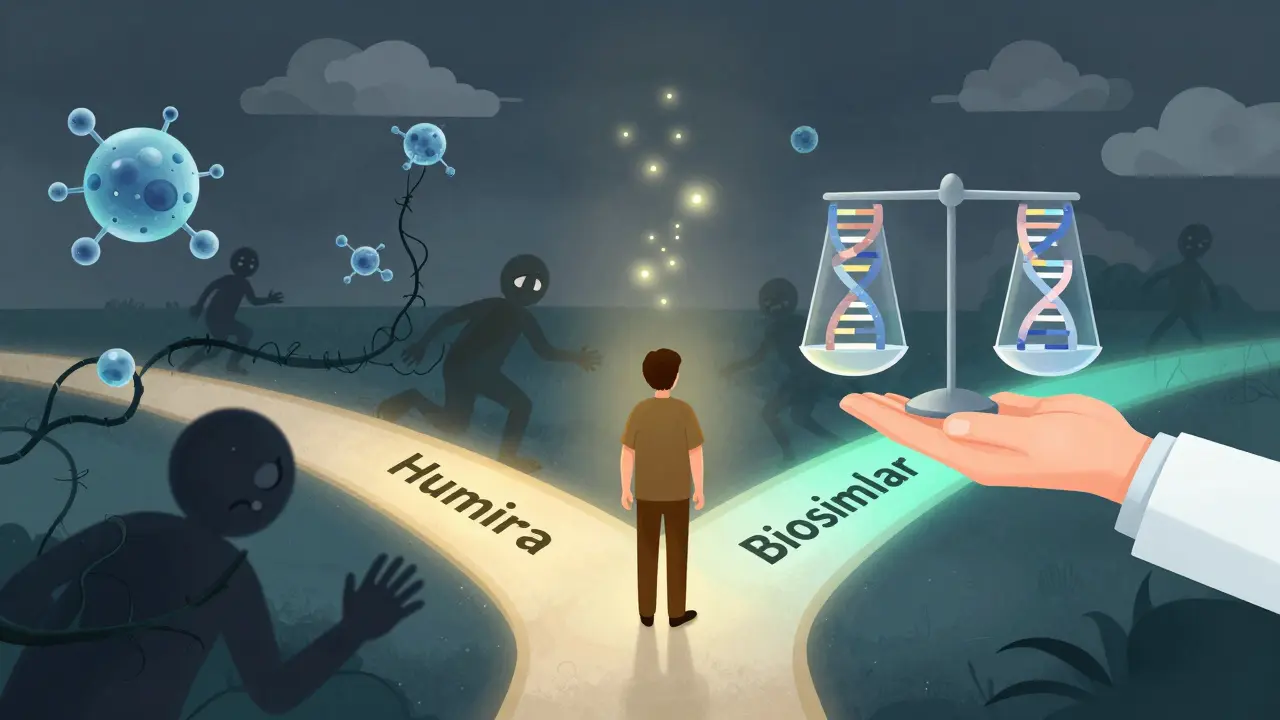
When your doctor says you can switch from Humira to a biosimilar, your first thought might not be savings-it might be fear. Biosimilars aren’t like generics. You can’t just swap them like you would ibuprofen for naproxen. They’re made from living cells, not chemicals. And that complexity is why so many patients hesitate-even when they could save hundreds or even thousands of dollars per year.
Why Biosimilars Feel Scary (Even When They’re Safe)
Most people understand generics. They’re cheaper versions of pills like metformin or lisinopril. Same active ingredient. Same effect. Same risk. But biosimilars? They’re different. They’re not exact copies. They’re highly similar-so similar that the FDA says there’s no meaningful difference in how they work or how safe they are. But that’s not how patients hear it. A 2025 survey from the Evernorth Research Institute found that only 31% of patients with chronic conditions even knew biosimilars existed. Meanwhile, 79% worried they wouldn’t work as well. Sixty-three percent feared new or worse side effects. One Reddit user, ChronicPainPatient87, shared how a switch to a biosimilar without warning led to a flare-up. He didn’t know it was a biosimilar until after. Now he refuses to try another. That’s not just fear. That’s trauma. And it’s not rare. When patients feel left out of the decision, trust breaks. And once trust is gone, even the most scientifically sound option feels risky.Biosimilars vs Generics: The Real Difference
Let’s clear up the biggest confusion: biosimilars are not generics. They can’t be. Generics are made from simple chemical formulas. Think aspirin or antibiotics. Once the patent expires, any lab can recreate the molecule exactly. The FDA only needs to prove it’s the same chemical. That takes about 3-4 years and costs $2-3 million. Biosimilars? They come from living cells-human or animal cells grown in bioreactors. Tiny changes in temperature, nutrients, or handling can alter the final product. Even small differences in structure might affect how the body reacts. That’s why developers must run hundreds of lab tests, animal studies, and at least one clinical trial to prove they behave just like the original drug. It takes 8-10 years. Costs $100-250 million. The FDA doesn’t approve biosimilars because they’re cheaper. They approve them because they’re just as safe and effective. Over 74 biosimilars have been approved in the U.S. since 2015. And data from real-world use shows no increase in side effects or treatment failures compared to the original biologics. But patients don’t see that data. They see the word “similar” and think “not the same.”Why Don’t Patients Save Money Even When Biosimilars Are Cheaper?
Here’s the frustrating part: biosimilars can cut drug costs by 35% on average. For pegfilgrastim, out-of-pocket costs dropped 47-59% in the first cycle. But here’s what happens next: many patients still pay the same. Why? Because pharmacy benefit managers (PBMs) and insurers don’t always pass savings along. In many cases, the biosimilar is priced lower-but the patient’s copay stays locked at the same level as the original drug. A 2025 study found that for infliximab, patient costs didn’t drop even after biosimilars entered the market. When CVS removed Humira from most commercial formularies in April 2024, the average cost of biologics dropped by 2.3 percentage points. But patient satisfaction fell by 15%. Why? Because patients felt forced into a switch they didn’t understand. The system saved money. But the patient felt punished. True savings mean lower out-of-pocket costs. Without that, even the best science won’t win trust.
What Doctors Aren’t Telling You (And Why)
Many physicians want to prescribe biosimilars. But they’re caught in the middle. Only 68-88% of healthcare providers feel confident explaining biosimilars to patients, according to the Center for Biosimilars. Some don’t know the latest data. Others worry about liability. A few still believe biosimilars are “second-rate.” And when a doctor says, “This is just like your old medicine,” patients hear, “They’re cutting corners.” The solution isn’t more jargon. It’s transparency. Doctors need to say: “This isn’t a generic. It’s a biosimilar. It’s made differently, but it works the same. Here’s what we know from studies and real-world use.” One clinic in Minnesota started showing patients actual lab reports-comparing antibody levels and disease markers before and after switching. Patients saw their own data. No fluff. Just facts. Within six months, refusal rates dropped from 40% to 12%.How to Build Trust: Real Steps for Patients and Providers
If you’re a patient who’s been asked to switch:- Ask: “Is this a biosimilar? How is it different from my current drug?”
- Ask: “Will my out-of-pocket cost go down?”
- Ask: “Can I see data on how this has worked for other people with my condition?”
- Don’t assume patients know what biosimilars are. Explain them like you would a new treatment.
- Use visual aids-charts showing similar efficacy rates, side effect profiles, or cost comparisons.
- Never switch without consent. Give patients time to ask questions.
- Track real-world outcomes: monitor disease activity, lab values, and patient-reported symptoms. Share those results with them.
What’s Changing Now-and What’s Coming
The FDA’s 2024 draft guidance is a big deal. It says manufacturers may no longer need to run full clinical trials for every biosimilar. Instead, they can rely on deep analytical testing. That could speed up approvals and bring more options to market faster. By 2034, nearly $232 billion in U.S. biologic sales will lose exclusivity. That means hundreds of new biosimilars could enter the market. But only if patients trust them. The biggest barrier isn’t science. It’s communication. And it’s not about convincing people to take cheaper drugs. It’s about helping them feel safe, informed, and in control. Right now, only 21% of patients say they have strong knowledge about biosimilars. But Dr. Lisa Chen from Evernorth predicts that by 2030, adoption will exceed 50%-if we stop treating patients like numbers and start treating them like partners.What You Can Do Today
You don’t need to wait for policy changes or new guidelines. You can start now:- If you’re on a biologic and your insurance suggests a switch, ask for the name of the biosimilar. Look it up. Check the FDA’s list of approved biosimilars.
- Ask your pharmacist: “Will this change my cost? Will I need to do anything different?”
- If you’ve had a bad experience, tell your doctor. Your story matters.
- Share your experience-positively or negatively. Real stories change minds more than brochures.
Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original biologic. Thousands of patients have used biosimilars since 2015, and real-world data shows no increase in side effects or treatment failures. Studies track antibody levels, disease markers, and hospitalization rates-all showing equivalent outcomes.
Why are biosimilars cheaper if they’re so complex to make?
Biosimilars are cheaper because they don’t need to repeat the original clinical trials. The reference drug already proved safety and effectiveness. Biosimilar makers only need to show they’re highly similar, which cuts development time and cost by up to 90%. That savings gets passed to the system-but not always to the patient. When insurers and PBMs lower list prices, patients should see lower copays. If they don’t, it’s a system issue, not a product issue.
Can I switch back to the original drug if the biosimilar doesn’t work for me?
Yes. Switching is not permanent. If you experience a flare-up, increased side effects, or any concern, talk to your doctor. You can return to the original biologic. Many patients who initially hesitated have switched back and then re-switched successfully after gaining confidence. What matters is communication-not just the drug name.
Why don’t I save money even though biosimilars cost less?
Insurance plans and pharmacy benefit managers (PBMs) sometimes set the same copay for both the original and biosimilar, even when the biosimilar is cheaper. This is a pricing strategy, not a scientific one. Ask your pharmacist or insurer: “Is my copay based on the biosimilar’s lower price?” If not, request a review. Some states are now requiring transparency in how copays are calculated.
How do I know if my drug has a biosimilar?
Check the FDA’s official list of approved biosimilars at fda.gov/biosimilars. You can search by brand name (like Humira, Enbrel, or Remicade). If a biosimilar exists, your pharmacy or insurer may notify you. But don’t wait for them-ask your doctor or pharmacist directly. If you’re on a biologic, it’s worth asking if a biosimilar option is available.

Curtis Younker
Man, I wish more docs would just sit down and talk like humans instead of dumping jargon on us. I switched to a biosimilar last year after my insurance forced it, and yeah, I was scared as hell. But my rheumatologist showed me my own lab results before and after - same inflammation markers, same energy levels. No magic, no snake oil. Just science that works. And I saved $800 a month. That’s a vacation. That’s groceries. That’s not getting evicted. Stop treating us like we’re dumb. We just want to know what’s happening to our bodies.
And yeah, PBMs are the real villains here. Why does my copay stay the same when the drug costs half? That’s not healthcare - that’s corporate theater. Fix the system, not just the script.
Shawn Raja
So let me get this straight - we’ve got a drug made from living cells, costing $200M to develop, approved by the FDA as functionally identical… but patients are scared because the word ‘similar’ sounds like ‘kinda sorta maybe’? Meanwhile, we’ll gladly swallow a generic pill labeled ‘same as aspirin’ but won’t trust a biosimilar because it’s ‘not exactly the same’?
That’s not fear of the unknown. That’s the human brain screaming at complexity. We’d rather die of inflammation than admit we don’t understand bioreactors. The real biosimilar here? Our collective refusal to evolve beyond 1950s medicine logic. We want our drugs to be like soda cans - identical, stackable, boring. But life doesn’t work that way. Neither do proteins.
Also, if your copay didn’t drop, blame your insurer, not the molecule. It’s not the biosimilar’s fault your healthcare is a rigged game.
Rakesh Kakkad
It is imperative to recognize that biosimilars are not merely pharmaceutical alternatives; they represent a paradigm shift in global healthcare economics. The regulatory frameworks established by the FDA are scientifically rigorous and globally aligned with EMA and WHO standards. The apprehension expressed by certain patient populations stems not from scientific inadequacy, but from a systemic failure in health literacy dissemination. It is therefore the moral and professional obligation of healthcare providers to elucidate the molecular and immunological equivalence through evidence-based, non-technical communication. The absence of such dialogue constitutes a breach of the patient-provider fiduciary relationship.
Nicholas Miter
i’ve been on humira since 2018. switched to a biosimilar last year after my insurance kicked me off. was nervous. didn’t tell anyone. checked my blood work after 3 months - same numbers. no new rashes, no flares. honestly? i didn’t even notice the difference. my doc didn’t push it. just said, ‘here’s what’s changing, here’s what’s not, here’s how to tell if something’s off.’ that’s all i needed.
also, my copay went from $120 to $40. so… yeah. the system’s broken, but the drug? it’s fine.
Suresh Kumar Govindan
The FDA’s approval process is a charade. Biosimilars are not equivalent. The complexity of protein folding cannot be replicated with statistical confidence. The clinical trials are underpowered, the sample sizes are laughable, and the post-marketing surveillance is nonexistent. This is not medicine - it is corporate cost-cutting disguised as innovation. You are being used as test subjects. Do not trust the system.
TONY ADAMS
bro my cousin switched and got super sick. like, threw up for a week. now she’s back on humira. biosimilars are just cheap knockoffs. why would you risk your life for $50 a month? the company’s just trying to make more money. don’t be a lab rat.
Ashley Karanja
Okay, but let’s talk about the emotional labor here - because this isn’t just about pharmacokinetics. It’s about the trauma of being switched without consent, the gaslighting when you say ‘I feel different,’ the dismissal when you say ‘I need to know what I’m getting.’ I’m a nurse, and I’ve seen patients cry because they were told, ‘It’s the same thing.’ But it’s not the same thing when your body remembers the old one. We need to normalize asking, ‘Can I try it with support?’ Not ‘You have to switch.’
And honestly? The fact that we’re still having this conversation in 2025? That’s the real failure. We have the data. We have the tools. We just don’t have the empathy.
Shweta Deshpande
I was skeptical too - I’ve been on Enbrel for 12 years. But my doctor gave me a folder with before-and-after lab reports from 30 other patients with my exact condition. Saw my own numbers in the same chart. No hype. Just graphs. I thought, ‘If it worked for them, why not me?’
Switched. No issues. Saved $600/month. My kid got a new bike. My mom stopped worrying. I didn’t lose anything except my fear. And honestly? That was the heaviest thing to carry.
Don’t let fear write your story. Ask questions. Get data. Talk to others. You’re not alone in this.
Josh josh
so i switched to the biosimilar and my doc never even told me it was one until i checked the bottle. like wtf. now i feel like i got scammed. also my copay didnt drop. this system is rigged. just sayin.
bella nash
It is noteworthy that the pharmacological equivalence of biosimilars is predicated upon a narrow set of analytical parameters, which, while statistically significant, may not fully capture the heterogeneity of biological response across diverse patient populations. The regulatory paradigm, though ostensibly robust, remains fundamentally reductionist in its approach to complex physiological systems. One must therefore remain vigilant against the conflation of regulatory approval with clinical infallibility.
Geoff Miskinis
Let’s be brutally honest - the only reason biosimilars exist is because Big Pharma realized they could milk the same patent cliff twice. First by charging $70K/year for Humira. Then by selling a ‘similar’ version for $45K and pretending it’s a win for patients. The real savings? Went to shareholders. The real risk? Went to you. And now we’re supposed to applaud the fact that your copay didn’t change? Pathetic.
Sally Dalton
my heart just broke reading about ChronicPainPatient87. i’ve been there. switched without warning, felt awful for weeks, thought i was dying. turned out it was just my body adjusting - but no one told me that. i cried in the pharmacy parking lot. if you’re a doc reading this: please, please, please don’t just say ‘it’s the same.’ say ‘this is different, but here’s how it’s the same, and here’s what to watch for.’
we’re not stubborn. we’re scared. and we just need someone to hold our hand while we take the leap.
Betty Bomber
i’ve been on a biosimilar for 2 years. no issues. saved money. doc didn’t make a big deal. i didn’t make a big deal. life went on. sometimes the simplest thing is the right thing.
Mohammed Rizvi
you know what’s wild? people freak out about biosimilars but will take a $20 supplement from a guy on YouTube who says ‘it’s made in a lab with quantum energy.’
we trust snake oil influencers but not FDA-approved science? that’s not fear of medicine - that’s fear of being lied to by the system. and honestly? we’ve got a right to be.
eric fert
Let’s not pretend this is about patient safety. This is about the pharmaceutical-industrial complex needing to replace their $70,000/year biologics with $45,000 versions so they can keep their profit margins while pretending they’re ‘helping’ patients. The FDA approves biosimilars because they’re cheaper to regulate - not because they’re more beneficial. And the real tragedy? Patients who actually feel worse after switching are told they’re ‘imagining it.’ That’s not science. That’s gaslighting dressed in a white coat.
And don’t even get me started on PBMs. They’re the real monsters. They set the copay so high that patients pay the same whether they get the original or the biosimilar. That’s not innovation. That’s theft. And we’re all just supposed to nod and say ‘thank you for the savings’ while our wallets stay empty and our bodies suffer.