Dyspareunia: Causes, Treatments, and What You Can Do About Painful Sex
When sex hurts, it’s not just physical—it affects your confidence, your relationship, and your sense of well-being. Dyspareunia, the medical term for persistent or recurrent pain during sexual intercourse. Also known as painful intercourse, it affects women of all ages and isn’t something you just have to live with. This isn’t rare. Studies show up to 1 in 5 women experience it at some point, yet most wait months—or years—before seeking help because they think it’s normal or embarrassing.
Dyspareunia isn’t one thing. It can come from multiple places: dryness after menopause, infections like yeast or bacterial vaginosis, scar tissue from childbirth or surgery, or even muscle tightness in the pelvic floor. Sometimes it’s tied to conditions like endometriosis or vulvodynia, where the nerves in the vulvar area become over-sensitive. And yes, stress and anxiety can make it worse—your body doesn’t separate emotional and physical pain. Pelvic floor dysfunction, when the muscles around your pelvis are too tight or don’t relax properly. Also known as vaginismus, it’s a common but often misdiagnosed cause of dyspareunia. Then there’s hormonal changes, especially drops in estrogen after childbirth or during menopause. Also known as atrophic vaginitis, this leads to thinning, dry tissue that tears easily during sex. These aren’t just side effects—they’re treatable conditions.
What you’ll find in the posts below isn’t a list of generic advice. It’s real, practical comparisons from people who’ve been there: how birth control pills like Yasmin can affect vaginal dryness, how blood pressure meds like metoprolol might impact sexual response, how topical treatments like diclofenac gel help with localized pain, and how antidepressants like sertraline can both help and hurt depending on the person. These aren’t random posts—they’re connected by one truth: dyspareunia doesn’t happen in a vacuum. It’s shaped by your hormones, your medications, your mental health, and your body’s response to stress. The goal here isn’t to scare you. It’s to give you the tools to talk to your doctor, ask the right questions, and finally find relief—not just a temporary fix, but a real solution.
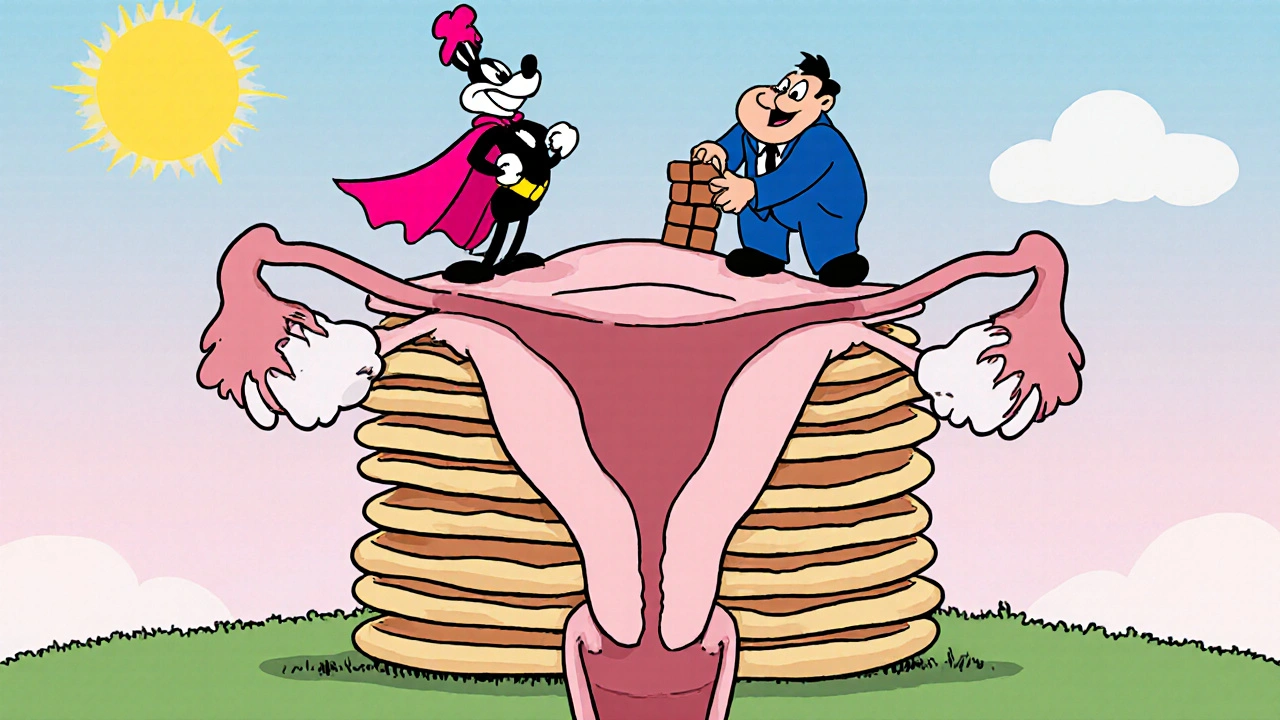
Uterine Lining Overgrowth and Its Impact on Your Sex Life
Learn how a thickened uterine lining (endometrial hyperplasia) can cause pain, dryness, and low libido, and discover diagnosis steps, treatment options, and tips to protect your sex life.
More