Alcohol Interaction: What You Need to Know About Mixing Drinks and Medications
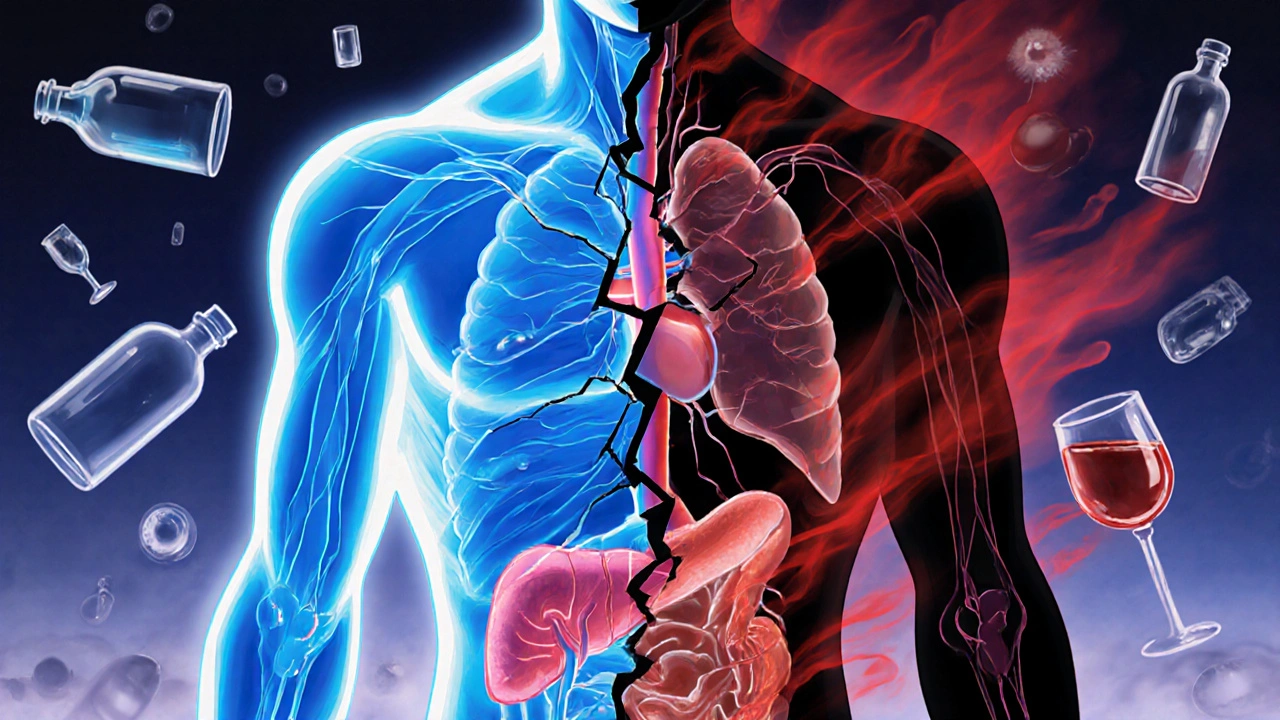
When you mix alcohol interaction, the way alcohol changes how your body handles medications. Also known as drug-alcohol interactions, it’s not just about feeling dizzy—it can stop your medicine from working, overload your liver, or even stop your breathing. This isn’t a myth. It’s a real risk millions face every day, often without knowing it.
Take warfarin, a blood thinner that’s sensitive to even small changes in diet and lifestyle. A few drinks can make it too strong, raising your risk of bleeding. Or consider antidepressants, medications that already affect brain chemistry. Alcohol can make them less effective—or turn mild side effects like drowsiness into dangerous dizziness. Even something as simple as ibuprofen, a common painkiller, becomes riskier with alcohol. Together, they can wreck your stomach lining or stress your kidneys. These aren’t rare cases. They’re common enough that doctors ask about drinking habits during every medication review.
It’s not just prescription drugs. Over-the-counter cold meds, sleep aids, and even herbal supplements like St. John’s Wort can turn dangerous when paired with alcohol. Some interactions show up right away—nausea, confusion, fainting. Others creep in slowly: liver damage, mood swings, or worsening anxiety. The real problem? Most people don’t realize their medicine has a warning label for alcohol. They think, "It’s just one glass," or "I took it hours ago." But alcohol doesn’t wait for you to finish drinking before it starts messing with your pills. It’s in your system, working side by side with your medication, often without you noticing.
If you’re on any regular medication, alcohol interaction isn’t something you can guess your way through. It’s not about being perfect—it’s about being informed. You don’t need to give up drinks entirely, but you do need to know which combinations are safe and which aren’t. Below, you’ll find real stories and clear breakdowns from people who’ve been there: the woman who almost bled out after a glass of wine with her blood thinner, the man who thought his sleep meds were failing until he stopped drinking, the parent who caught a dangerous double dose in their child’s cold syrup because they didn’t check for hidden alcohol. These aren’t edge cases. They’re warnings written in real life. And they’re here to help you avoid the same mistakes.
Trimethoprim and Alcohol: What You Need to Know About the Risks
Mixing trimethoprim and alcohol can worsen side effects, slow recovery, and trigger dangerous reactions. Learn the real risks and what to do if you’ve already had a drink.
More